Glycogen storage disease type I
Encyclopedia
Glycogen storage disease type I (GSD I) or von Gierke's disease, is the most common of the glycogen storage disease
Glycogen storage disease
Glycogen storage disease is the result of defects in the processing of glycogen synthesis or breakdown within muscles, liver, and other cell types. GSD has two classes of cause: genetic and acquired. Genetic GSD is caused by any inborn error of metabolism involved in these processes...
s. This genetic disease results from deficiency of the enzyme
Enzyme
Enzymes are proteins that catalyze chemical reactions. In enzymatic reactions, the molecules at the beginning of the process, called substrates, are converted into different molecules, called products. Almost all chemical reactions in a biological cell need enzymes in order to occur at rates...
glucose-6-phosphatase. This deficiency impairs the ability of the liver
Liver
The liver is a vital organ present in vertebrates and some other animals. It has a wide range of functions, including detoxification, protein synthesis, and production of biochemicals necessary for digestion...
to produce free glucose
Glucose
Glucose is a simple sugar and an important carbohydrate in biology. Cells use it as the primary source of energy and a metabolic intermediate...
from glycogen
Glycogen
Glycogen is a molecule that serves as the secondary long-term energy storage in animal and fungal cells, with the primary energy stores being held in adipose tissue...
and from gluconeogenesis
Gluconeogenesis
Gluconeogenesis is a metabolic pathway that results in the generation of glucose from non-carbohydrate carbon substrates such as lactate, glycerol, and glucogenic amino acids....
. Since these are the two principal metabolic
Metabolism
Metabolism is the set of chemical reactions that happen in the cells of living organisms to sustain life. These processes allow organisms to grow and reproduce, maintain their structures, and respond to their environments. Metabolism is usually divided into two categories...
mechanisms by which the liver supplies glucose to the rest of the body during periods of fasting
Fasting
Fasting is primarily the act of willingly abstaining from some or all food, drink, or both, for a period of time. An absolute fast is normally defined as abstinence from all food and liquid for a defined period, usually a single day , or several days. Other fasts may be only partially restrictive,...
, it causes severe hypoglycemia
Hypoglycemia
Hypoglycemia or hypoglycæmia is the medical term for a state produced by a lower than normal level of blood glucose. The term literally means "under-sweet blood"...
. Reduced glycogen breakdown results in increased glycogen storage in liver and kidneys, causing enlargement of both. Both organs function normally in childhood but are susceptible to a variety of problems in the adult years. Other metabolic derangements include lactic acidosis
Lactic acidosis
Lactic acidosis is a physiological condition characterized by low pH in body tissues and blood accompanied by the buildup of lactate especially D-lactate, and is considered a distinct form of metabolic acidosis. The condition typically occurs when cells receive too little oxygen , for example...
and hyperlipidemia
Hyperlipidemia
Hyperlipidemia, hyperlipoproteinemia, or hyperlipidaemia is the condition of abnormally elevated levels of any or all lipids and/or lipoproteins in the blood...
. Frequent or continuous feedings of cornstarch
Cornstarch
Corn starch, cornstarch, cornflour or maize starch is the starch of the corn grain obtained from the endosperm of the corn kernel.-History:...
or other carbohydrate
Carbohydrate
A carbohydrate is an organic compound with the empirical formula ; that is, consists only of carbon, hydrogen, and oxygen, with a hydrogen:oxygen atom ratio of 2:1 . However, there are exceptions to this. One common example would be deoxyribose, a component of DNA, which has the empirical...
s are the principal treatment. Other therapeutic measures may be needed for associated problems.
The disease is named after Edgar von Gierke
Edgar von Gierke
Edgar Otto Conrad von Gierke was a German doctor, who specialised in glycogen synthesis. This research led him to the discovery of glycogen synthesis type I.He married Julie Brown in 1912 and fathered 4 children....
, the German doctor who discovered it.
Molecular biology
Glucose-6-phosphatase is an enzyme located on the inner membraneBiological membrane
A biological membrane or biomembrane is an enclosing or separatingmembrane that acts as a selective barrier, within or around a cell. It consists of a lipid bilayer with embedded proteins that may constitute close to 50% of membrane content...
of the endoplasmic reticulum
Endoplasmic reticulum
The endoplasmic reticulum is an organelle of cells in eukaryotic organisms that forms an interconnected network of tubules, vesicles, and cisternae...
. The catalytic unit
Catalysis
Catalysis is the change in rate of a chemical reaction due to the participation of a substance called a catalyst. Unlike other reagents that participate in the chemical reaction, a catalyst is not consumed by the reaction itself. A catalyst may participate in multiple chemical transformations....
is associated with a calcium
Calcium
Calcium is the chemical element with the symbol Ca and atomic number 20. It has an atomic mass of 40.078 amu. Calcium is a soft gray alkaline earth metal, and is the fifth-most-abundant element by mass in the Earth's crust...
binding protein
Protein
Proteins are biochemical compounds consisting of one or more polypeptides typically folded into a globular or fibrous form, facilitating a biological function. A polypeptide is a single linear polymer chain of amino acids bonded together by peptide bonds between the carboxyl and amino groups of...
, and three transport proteins (T1, T2, T3) that facilitate movement of glucose-6-phosphate (G6P), glucose
Glucose
Glucose is a simple sugar and an important carbohydrate in biology. Cells use it as the primary source of energy and a metabolic intermediate...
, and phosphate
Phosphate
A phosphate, an inorganic chemical, is a salt of phosphoric acid. In organic chemistry, a phosphate, or organophosphate, is an ester of phosphoric acid. Organic phosphates are important in biochemistry and biogeochemistry or ecology. Inorganic phosphates are mined to obtain phosphorus for use in...
(respectively) into and out of the enzyme.
The most common forms of GSD I are designated GSD Ia and GSD Ib, the former accounting for over 80% of diagnosed cases and the latter for less than 20%. A few rarer forms have been described.
- GSD Ia results from mutations of G6PC, the geneGeneA gene is a molecular unit of heredity of a living organism. It is a name given to some stretches of DNA and RNA that code for a type of protein or for an RNA chain that has a function in the organism. Living beings depend on genes, as they specify all proteins and functional RNA chains...
for glucose-6-phosphatase. G6PC is located on chromosomeChromosomeA chromosome is an organized structure of DNA and protein found in cells. It is a single piece of coiled DNA containing many genes, regulatory elements and other nucleotide sequences. Chromosomes also contain DNA-bound proteins, which serve to package the DNA and control its functions.Chromosomes...
17q21. - GSD Ib results from mutations of the gene for SLC37A4SLC37A4Glucose-6-phosphate translocase is an enzyme that in humans is encoded by the SLC37A4 gene.-Further reading:...
or "G6PT1", the G6P transporter. - GSD Ic results from mutations of SLC17A3 or SLC37A4SLC37A4Glucose-6-phosphate translocase is an enzyme that in humans is encoded by the SLC37A4 gene.-Further reading:...
.
The metabolic characteristics of GSD Ia and Ib are quite similar, but Ib incurs a few additional problems (described below).
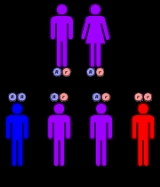
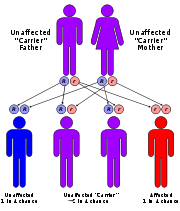
Genetic prevalence
Prenatal diagnosis
Prenatal diagnosis or prenatal screening is testing for diseases or conditions in a fetus or embryo before it is born. The aim is to detect birth defects such as neural tube defects, Down syndrome, chromosome abnormalities, genetic diseases and other conditions, such as spina bifida, cleft palate,...
has been made by fetal liver biopsy
Liver biopsy
Liver biopsy is the biopsy from the liver. It is a medical test that is done to aid diagnosis of liver disease, to assess the severity of known liver disease, and to monitor the progress of treatment.-History:...
at 18–22 weeks of gestation, but no fetal treatment has been proposed. Prenatal diagnosis is possible with fetal DNA
DNA
Deoxyribonucleic acid is a nucleic acid that contains the genetic instructions used in the development and functioning of all known living organisms . The DNA segments that carry this genetic information are called genes, but other DNA sequences have structural purposes, or are involved in...
obtained by chorionic villus sampling
Chorionic villus sampling
Chorionic villus sampling , sometimes misspelled "chorionic villous sampling", is a form of prenatal diagnosis to determine chromosomal or genetic disorders in the fetus. It entails sampling of the chorionic villus and testing it...
when a fetus is known to be at risk.
GSD Ia has an incidence
Incidence (epidemiology)
Incidence is a measure of the risk of developing some new condition within a specified period of time. Although sometimes loosely expressed simply as the number of new cases during some time period, it is better expressed as a proportion or a rate with a denominator.Incidence proportion is the...
in the American population of approximately 1 in 50,000 to 100,000 births. None of the glycogenoses are currently detected by standard or extended newborn screening
Newborn screening
Newborn screening is the process by which infants are screened shortly after birth for a list of disorders that are treatable, but difficult or impossible to detect clinically. Screening programs are often run by state or national governing bodies with the goal of screening all infants born in the...
.
Normal carbohydrate balance and maintenance of blood glucose levels
Glycogen in liver and (to a lesser degree) kidneys serves as a form of stored, rapidly accessible glucose, so that the blood glucose level can be maintained between meals. For about 3 hours after a carbohydrate-containing meal, high insulin levels direct liver cells to take glucose from the blood, to convert it to glucose-6-phosphate (G6P), and to add the G6P molecules to the ends of chains of glycogen (glycogen synthesis). Excess G6P is also shunted into production of triglycerideTriglyceride
A triglyceride is an ester derived from glycerol and three fatty acids. There are many triglycerides, depending on the oil source, some are highly unsaturated, some less so....
s and exported for storage in adipose tissue
Adipose tissue
In histology, adipose tissue or body fat or fat depot or just fat is loose connective tissue composed of adipocytes. It is technically composed of roughly only 80% fat; fat in its solitary state exists in the liver and muscles. Adipose tissue is derived from lipoblasts...
as fat
Fat
Fats consist of a wide group of compounds that are generally soluble in organic solvents and generally insoluble in water. Chemically, fats are triglycerides, triesters of glycerol and any of several fatty acids. Fats may be either solid or liquid at room temperature, depending on their structure...
.
When digestion
Digestion
Digestion is the mechanical and chemical breakdown of food into smaller components that are more easily absorbed into a blood stream, for instance. Digestion is a form of catabolism: a breakdown of large food molecules to smaller ones....
of a meal is complete, insulin levels fall, and enzyme systems in the liver cells begin to remove glucose molecules from strands of glycogen in the form of G6P. This process is termed glycogenolysis
Glycogenolysis
Glycogenolysis is the conversion of glycogen polymers to glucose monomers. Glycogen is catabolized by removal of a glucose monomer through cleavage with inorganic phosphate to produce glucose-1-phosphate...
. The G6P remains within the liver cell unless the phosphate is cleaved by glucose-6-phosphatase. This dephosphorylation
Dephosphorylation
Dephosphorylation is the essential process of removing phosphate groups from an organic compound by hydrolysis. Its opposite is phosphorylation...
reaction produces free glucose and free PO4 anions. The free glucose molecules can be transported out of the liver cells into the blood to maintain an adequate supply of glucose to the brain
Brain
The brain is the center of the nervous system in all vertebrate and most invertebrate animals—only a few primitive invertebrates such as sponges, jellyfish, sea squirts and starfishes do not have one. It is located in the head, usually close to primary sensory apparatus such as vision, hearing,...
and other organs of the body. Glycogenolysis can supply the glucose needs of an adult body for 12–18 hours.
When fasting continues for more than a few hours, falling insulin levels permit catabolism
Catabolism
Catabolism is the set of metabolic pathways that break down molecules into smaller units and release energy. In catabolism, large molecules such as polysaccharides, lipids, nucleic acids and proteins are broken down into smaller units such as monosaccharides, fatty acids, nucleotides, and amino...
of muscle
Muscle
Muscle is a contractile tissue of animals and is derived from the mesodermal layer of embryonic germ cells. Muscle cells contain contractile filaments that move past each other and change the size of the cell. They are classified as skeletal, cardiac, or smooth muscles. Their function is to...
protein and triglycerides from adipose tissue. The products of these processes are amino acid
Amino acid
Amino acids are molecules containing an amine group, a carboxylic acid group and a side-chain that varies between different amino acids. The key elements of an amino acid are carbon, hydrogen, oxygen, and nitrogen...
s (mainly alanine
Alanine
Alanine is an α-amino acid with the chemical formula CH3CHCOOH. The L-isomer is one of the 20 amino acids encoded by the genetic code. Its codons are GCU, GCC, GCA, and GCG. It is classified as a nonpolar amino acid...
), free fatty acids, and lactic acid
Lactic acid
Lactic acid, also known as milk acid, is a chemical compound that plays a role in various biochemical processes and was first isolated in 1780 by the Swedish chemist Carl Wilhelm Scheele. Lactic acid is a carboxylic acid with the chemical formula C3H6O3...
. Free fatty acids from triglycerides are converted to ketone
Ketone
In organic chemistry, a ketone is an organic compound with the structure RCR', where R and R' can be a variety of atoms and groups of atoms. It features a carbonyl group bonded to two other carbon atoms. Many ketones are known and many are of great importance in industry and in biology...
s, and to acetyl-CoA
Acetyl-CoA
Acetyl coenzyme A or acetyl-CoA is an important molecule in metabolism, used in many biochemical reactions. Its main function is to convey the carbon atoms within the acetyl group to the citric acid cycle to be oxidized for energy production. In chemical structure, acetyl-CoA is the thioester...
. Amino acids and lactic acid are used to synthesize new G6P in liver cells by the process of gluconeogenesis
Gluconeogenesis
Gluconeogenesis is a metabolic pathway that results in the generation of glucose from non-carbohydrate carbon substrates such as lactate, glycerol, and glucogenic amino acids....
. The last step of normal gluconeogenesis, like the last step of glycogenolysis, is the dephosphorylation of G6P by glucose-6-phosphatase to free glucose and PO4.
Thus glucose-6-phosphatase mediates the final, key, step in both of the two main processes of glucose production during fasting. In fact the effect is amplified because the resulting high levels of glucose-6-phosphate inhibit earlier key steps in both glycogenolysis and gluconeogenesis.
Pathophysiology
The principal metabolic effects of deficiency of glucose-6-phosphatase are:- hypoglycemiaHypoglycemiaHypoglycemia or hypoglycæmia is the medical term for a state produced by a lower than normal level of blood glucose. The term literally means "under-sweet blood"...
- lactic acidosisLactic acidosisLactic acidosis is a physiological condition characterized by low pH in body tissues and blood accompanied by the buildup of lactate especially D-lactate, and is considered a distinct form of metabolic acidosis. The condition typically occurs when cells receive too little oxygen , for example...
- hypertriglyceridemiaHypertriglyceridemiaIn medicine, hypertriglyceridemia denotes high blood levels of triglycerides, the most abundant fatty molecule in most organisms. It has been associated with atherosclerosis, even in the absence of hypercholesterolemia . It can also lead to pancreatitis in excessive concentrations In medicine,...
- hyperuricemiaHyperuricemiaHyperuricemia is a level of uric acid in the blood that is abnormally high. In humans, the upper end of the normal range is 360 µmol/L for women and 400 µmol/L for men.-Causes:...
The hypoglycemia of GSD I is termed "fasting", or "post-absorptive", meaning that it occurs after completion of digestion of a meal—usually about 4 hours later. This inability to maintain adequate blood glucose levels during fasting results from the combined impairment of both glycogenolysis and gluconeogenesis. Fasting hypoglycemia is often the most significant problem in GSD I, and typically the problem that leads to the diagnosis. Chronic hypoglycemia produces secondary metabolic adaptations, including chronically low insulin
Insulin
Insulin is a hormone central to regulating carbohydrate and fat metabolism in the body. Insulin causes cells in the liver, muscle, and fat tissue to take up glucose from the blood, storing it as glycogen in the liver and muscle....
levels and high levels of glucagon
Glucagon
Glucagon, a hormone secreted by the pancreas, raises blood glucose levels. Its effect is opposite that of insulin, which lowers blood glucose levels. The pancreas releases glucagon when blood sugar levels fall too low. Glucagon causes the liver to convert stored glycogen into glucose, which is...
and cortisol
Cortisol
Cortisol is a steroid hormone, more specifically a glucocorticoid, produced by the adrenal gland. It is released in response to stress and a low level of blood glucocorticoids. Its primary functions are to increase blood sugar through gluconeogenesis; suppress the immune system; and aid in fat,...
.
Lactic acidosis arises from impairment of gluconeogenesis. Lactic acid is generated both in the liver and muscle and is oxidized by NAD+ to pyruvic acid
Pyruvic acid
Pyruvic acid is an organic acid, a ketone, as well as the simplest of the alpha-keto acids. The carboxylate ion of pyruvic acid, CH3COCOO−, is known as pyruvate, and is a key intersection in several metabolic pathways....
and then converted via the gluconeogenenic pathway to G6P. Accumulation of G6P inhibits conversion of lactate to pyruvate. The lactic acid level rises during fasting as glucose falls. In people with GSD I, it may not fall entirely to normal even when normal glucose levels are restored.
Hypertriglyceridemia resulting from amplified triglyceride production is another indirect effect of impaired gluconeogenesis, amplified by chronically low insulin levels. During fasting, the normal conversion of triglycerides to free fatty acids, ketones, and ultimately glucose is impaired. Triglyceride levels in GSD I can reach several times normal and serve as a clinical index of "metabolic control".
Hyperuricemia results from a combination of increased generation and decreased excretion of uric acid
Uric acid
Uric acid is a heterocyclic compound of carbon, nitrogen, oxygen, and hydrogen with the formula C5H4N4O3. It forms ions and salts known as urates and acid urates such as ammonium acid urate. Uric acid is created when the body breaks down purine nucleotides. High blood concentrations of uric acid...
, which is generated when increased amounts of G6P are metabolized via the pentose phosphate pathway
Pentose phosphate pathway
The pentose phosphate pathway is a process that generates NADPH and pentoses . There are two distinct phases in the pathway. The first is the oxidative phase, in which NADPH is generated, and the second is the non-oxidative synthesis of 5-carbon sugars...
. It is also a byproduct of purine
Purine
A purine is a heterocyclic aromatic organic compound, consisting of a pyrimidine ring fused to an imidazole ring. Purines, including substituted purines and their tautomers, are the most widely distributed kind of nitrogen-containing heterocycle in nature....
degradation. Uric acid competes with lactic acid and other organic acids for renal excretion in the urine. In GSD I increased availability of G6P for the pentose phosphate pathway, increased rates of catabolism, and diminished urinary excretion due to high levels of lactic acid all combine to produce uric acid levels several times normal. Although hyperuricemia is asymptomatic for years, kidney and joint damage gradually accrue.
Principal clinical problems
Clinical manifestations result, directly or indirectly, from- inability to maintain an adequate blood glucose level during the post-absorptive hours of each day;
- organ changes due to glycogen accumulation;
- excessive lactic acid generation;
- damage to tissue from hyperuricemia;
- in GSD Ib, bleeding and infection risk from blood cell effects.
Hypoglycemia
HypoglycemiaHypoglycemia
Hypoglycemia or hypoglycæmia is the medical term for a state produced by a lower than normal level of blood glucose. The term literally means "under-sweet blood"...
is the central clinical problem, the one that is most damaging, and the one that most often prompts the initial diagnosis.
Maternal glucose transferred across the placenta
Placenta
The placenta is an organ that connects the developing fetus to the uterine wall to allow nutrient uptake, waste elimination, and gas exchange via the mother's blood supply. "True" placentas are a defining characteristic of eutherian or "placental" mammals, but are also found in some snakes and...
prevents hypoglycemia in a fetus with GSD I, but the liver is enlarged with glycogen at birth. The inability to generate and release glucose soon results in hypoglycemia, and occasionally in lactic acidosis fulminant enough to appear as a primary respiratory problem in the newborn period. Neurological manifestations are less severe than if the hypoglycemia were more acute. The brain's habituation to mild hypoglycemia is at least partly explained by use of alternative fuels, primarily lactate.
More commonly, infants with GSD I tolerate without obvious symptoms a chronic, mild hypoglycemia and compensated lactic acidosis between feedings. Blood glucose levels are typically 25 to 50 mg/dl (1.4-2.8 mM). These infants continue to need oral carbohydrates every few hours. Many never sleep through the night even in the second year of life. They may be pale, clammy, and irritable a few hours after a meal. Developmental delay is not an intrinsic or inevitable effect of glucose-6-phosphatase deficiency but is common if the diagnosis is not made in early infancy.
Although mild hypoglycemia for much of the day may go unsuspected, the metabolic adaptations described above make severe hypoglycemic episodes, with unconsciousness or seizure, uncommon before treatment. Episodes which occur are likely to happen in the morning before breakfast. GSD I is therefore a potential cause of ketotic hypoglycemia
Ketotic hypoglycemia
Ketotic hypoglycemia is a medical term used in two ways: broadly, to refer to any circumstance in which low blood glucose is accompanied by ketosis, and in a much more restrictive way to refer to recurrent episodes of hypoglycemic symptoms with ketosis and, often, vomiting, in young children...
in young children.
Once the diagnosis has been made, the principal goal of treatment is to maintain an adequate glucose level and prevent hypoglycemia.
Hepatomegaly and liver problems
Impairment of glycogenolysis also causes the characteristic enlargement of the liverHepatomegaly
Hepatomegaly is the condition of having an enlarged liver. It is a nonspecific medical sign having many causes, which can broadly be broken down into infection, direct toxicity, hepatic tumours, or metabolic disorder. Often, hepatomegaly will present as an abdominal mass...
due to accumulation of glycogen. Glycogen also accumulates in kidneys and small intestine. Hepatomegaly, usually without splenomegaly, begins to develop in fetal life and is usually noticeable in the first few months of life. By the time the child is standing and walking, the hepatomegaly may be severe enough to cause the abdomen to protrude. The liver edge is often at or below the level of the umbilicus
Navel
The navel is a scar on the abdomen caused when the umbilical cord is removed from a newborn baby...
. Other liver functions are usually spared, and liver enzymes and bilirubin
Bilirubin
Bilirubin is the yellow breakdown product of normal heme catabolism. Heme is found in hemoglobin, a principal component of red blood cells. Bilirubin is excreted in bile and urine, and elevated levels may indicate certain diseases...
are usually normal.
However, there is a risk of developing tumors of the liver by adolescence or adult ages, and periodic ultrasound examinations of the liver are recommended from late childhood onward. Occasional cases of various types of liver disease and failure have been reported in children and adults with GSD I.
Lactic acidosis
Impaired gluconeogenesis results in elevations of lactic acid (4-10 mM) even when the child is well. In an episode of metabolic decompensation, lactic acid levels abruptly rise and can exceed 15 mM, producing severe metabolic acidosis. Uric acid, ketoacids, and free fatty acids further increase the anion gapAnion gap
The anion gap is the difference in the measured cations and the measured anions in serum, plasma, or urine. The magnitude of this difference in the serum is often calculated in medicine when attempting to identify the cause of metabolic acidosis...
. Manifestations of severe metabolic acidosis include vomiting and hyperpnea
Hyperpnea
Hyperpnea or hyperpnoea is increased depth of breathing when required to meet metabolic demand of body tissues, such as during or following exercise, or when the body lacks oxygen , for instance in high altitude or as a result of anemia....
, which can exacerbate hypoglycemia by reducing oral intake. Repeated episodes of vomiting
Vomiting
Vomiting is the forceful expulsion of the contents of one's stomach through the mouth and sometimes the nose...
with hypoglycemia and dehydration
Dehydration
In physiology and medicine, dehydration is defined as the excessive loss of body fluid. It is literally the removal of water from an object; however, in physiological terms, it entails a deficiency of fluid within an organism...
may occur in infancy and childhood, precipitated by (or mimicking) infection
Infection
An infection is the colonization of a host organism by parasite species. Infecting parasites seek to use the host's resources to reproduce, often resulting in disease...
s such as gastroenteritis
Gastroenteritis
Gastroenteritis is marked by severe inflammation of the gastrointestinal tract involving both the stomach and small intestine resulting in acute diarrhea and vomiting. It can be transferred by contact with contaminated food and water...
or pneumonia
Pneumonia
Pneumonia is an inflammatory condition of the lung—especially affecting the microscopic air sacs —associated with fever, chest symptoms, and a lack of air space on a chest X-ray. Pneumonia is typically caused by an infection but there are a number of other causes...
.
Growth failure
Without treatment, growth failure is common, due to chronically low insulin levels, persistent acidosis, chronic elevation of catabolic hormones, calorieCalorie
The calorie is a pre-SI metric unit of energy. It was first defined by Nicolas Clément in 1824 as a unit of heat, entering French and English dictionaries between 1841 and 1867. In most fields its use is archaic, having been replaced by the SI unit of energy, the joule...
insufficiency, and/or malabsorption
Malabsorption
Malabsorption is a state arising from abnormality in absorption of food nutrients across the gastrointestinal tract.Impairment can be of single or multiple nutrients depending on the abnormality...
.
Hyperlipidemia and blood vessel effects
A secondary effect of low insulin levels is hypertriglyceridemia. Triglycerides in the 400–800 mg/dl range may produce visible lipemia, and even a mild pseudohyponatremia due to a reduced aqueous fraction of the serumBlood plasma
Blood plasma is the straw-colored liquid component of blood in which the blood cells in whole blood are normally suspended. It makes up about 55% of the total blood volume. It is the intravascular fluid part of extracellular fluid...
. Cholesterol
Cholesterol
Cholesterol is a complex isoprenoid. Specifically, it is a waxy steroid of fat that is produced in the liver or intestines. It is used to produce hormones and cell membranes and is transported in the blood plasma of all mammals. It is an essential structural component of mammalian cell membranes...
is only mildly elevated.
Hyperuricemia and joint problems
A further effect of chronic lactic acidosis in GSD I is hyperuricemia, as lactic acid and uric acid compete for the same renal tubular transport mechanism. Increased purine catabolism is an additional contributing factor. Uric acid levels of 6–12 mg/dl are typical of GSD I. Allopurinol may be needed to prevent uric acid nephropathy and gout.Kidney effects
Kidneys are usually 10 to 20% enlarged with stored glycogen. This does not usually cause clinical problems in childhood, with the occasional exception of a Fanconi syndromeFanconi syndrome
Falconi syndrome is a disease of the proximal renal tubules of the kidney in which glucose, amino acids, uric acid, phosphate and bicarbonate are passed into the urine, instead of being reabsorbed. Fanconi syndrome affects the proximal tubule, which is the first part of the tubule to process fluid...
with multiple derangements of renal tubular reabsorption, including proximal renal tubular acidosis with bicarbonate and phosphate wasting. However, prolonged hyperuricemia can cause uric acid nephropathy. In adults with GSD I, chronic glomerular damage similar to diabetic nephropathy may lead to renal failure.
Bowel effects
Intestinal involvement can cause mild malabsorptionMalabsorption
Malabsorption is a state arising from abnormality in absorption of food nutrients across the gastrointestinal tract.Impairment can be of single or multiple nutrients depending on the abnormality...
with sloppy stools but usually requires no treatment.
Infection risk
Neutropenia is a manifestation of this disease, GSCF therapy can improve the risk of infection.Blood clotting problems
Impaired platelet aggregation is an uncommon effect of chronic hypoglycemia. It may cause clinically significant bleeding, especially epistaxis.Neurodevelopmental effects
Developmental delay is a potential secondary effect of chronic or recurrent hypoglycemia, but is at least theoretically preventable. Because normal brain and muscle cells contain no glucose-6-phosphatase, GSD I causes no other neuromuscular effects.Presentation and diagnosis
Several different problems may lead to the diagnosis, usually by two years of age:- seizures or other manifestations of severe fasting hypoglycemia;
- hepatomegaly with abdominal protuberance;
- hyperventilation and apparent respiratory distress due to metabolic acidosis;
- episodes of vomiting due to metabolic acidosis, often precipitated by minor illness and accompanied by hypoglycemia.
Once the diagnosis is suspected, the multiplicity of clinical and laboratory features usually makes a strong circumstantial case. If hepatomegaly, fasting hypoglycemia, and poor growth are accompanied by lactic acidosis, hyperuricemia, hypertriglyceridemia, and enlarged kidneys by ultrasound, gsd I is the most likely diagnosis. The differential diagnosis list includes glycogenoses types III and VI, fructose 1,6-bisphosphatase deficiency, and a few other conditions (page 5), but none are likely to produce all of the features of gsd I.
The next step is usually a carefully monitored fast. Hypoglycemia often occurs within six hours. A critical blood specimen obtained at the time of hypoglycemia typically reveals a mild metabolic acidosis, high free fatty acids and beta-hydroxybutyrate, very low insulin levels, and high levels of glucagon, cortisol, and growth hormone. Administration of intramuscular or intravenous glucagon (0.25 to 1 mg, depending on age) or epinephrine produces little rise of blood sugar.
The diagnosis is definitively confirmed by liver biopsy with electron microscopy and assay of glucose-6-phosphatase activity in the tissue and/or specific gene testing, available in recent years.
Treatment
The primary treatment goal is prevention of hypoglycemia and the secondary metabolic derangements by frequent feedings of foods high in glucose or starch (which is readily digested to glucose). To compensate for the inability of the liver to provide sugar, the total amount of dietary carbohydrate should approximate the 24-hour glucose production rate. The diet should contain approximately 65-70% carbohydrate, 10-15% protein, and 20-25% fat. At least a third of the carbohydrates should be supplied through the night, so that a young child goes no more than 3–4 hours without carbohydrate intakeIn the last 30 years, two methods have been used to achieve this goal in young children: (1) continuous nocturnal gastric infusion of glucose or starch; and (2) night-time feedings of uncooked cornstarch. An elemental formula, glucose polymer, and/or cornstarch can be infused continuously through the night at a rate supplying 0.5-0.6 g/kg/h of glucose for an infant, or 0.3-0.4 for an older child. This method requires a nasogastric or gastrostomy tube and pump. Sudden death from hypoglycemia has occurred due to malfunction or disconnection, and periodic cornstarch feedings are now preferred to continuous infusion.
Cornstarch is an inexpensive way to provide gradually digested glucose. One tablespoon contains nearly 9 g carbohydrate (36 calories). Although it is safer, less expensive, and requires no equipment, this method does require that parents arise every 3–4 hours to administer the cornstarch. A typical requirement for a young child is 1.6 g/kg every 4 hours.
Long-term management should eliminate hypoglycemic symptoms and maintain normal growth. Treatment should achieve normal glucose, lactic acid, and electrolyte levels, and only mild elevations of uric acid and triglycerides.
Avoidance of other sugars
Intake of carbohydrates which must be converted to G6P to be utilized (e.g., galactose and fructose) should be minimized. Although elemental formulas are available for infants, many foods contain fructose or galactose in the forms of sucrose or lactose. Adherence becomes a contentious treatment issue after infancy.Other therapeutic measures
Persistent elevation of uric acid above 6.5 mg/dl warrants treatment with allopurinol to prevent uric acid deposition in kidneys and joints.Because of the potential for impaired platelet function, coagulation ability should be checked and the metabolic state normalized before surgery. Bleeding time may be normalized with 1–2 days of glucose loading, and improved with ddavp. During surgery, iv fluids should contain 10% dextrose and no lactate.
A patient with GSD, type 1b was treated with a liver transplant at UCSF Medical Center in 1993 that resulted in the resolution of hypoglycemic episodes and the need for the patient to stay away from natural sources of sugar. It is unknown if other patients have undergone this procedure.
Treatment of acute metabolic acidosis episodes
The most significant acute problem in childhood is a vulnerability to episodes of metabolic acidosis precipitated by minor illnesses. If a vomiting illness persists longer than 2–4 hours, the child should be seen and assessed for dehydration, acidosis, and hypoglycemia. If these are developing, intravenous fluids should be provided at a rate above maintenance. For mild acidosis, an effective fluid is 10% dextrose in ½ normal saline with 20 mEq/l KCl, but if acidosis is severe, 75-100 mEq/l NaHCO3 and 20 mEq/l of K acetate can be substituted for the NaCl and KCl.Natural history, prognosis, long term complications
Without adequate metabolic treatment, patients with gsd I have died in infancy or childhood of overwhelming hypoglycemia and acidosis. Those who survived were stunted in physical growth and delayed in puberty because of chronically low insulin levels. Mental retardation from recurrent, severe hypoglycemia is considered preventable with appropriate treatment.Hepatic complications have been serious in some patients. Adenomas of the liver can develop in the second decade or later, with a small chance of later malignant transformation to hepatoma or hepatic carcinomas (detectable by alpha-fetoprotein screening). Several children with advanced hepatic complications have improved after liver transplantation.
Additional problems reported in adolescents and adults with gsd I have included hyperuricemic gout, pancreatitis, and chronic renal failure. Despite hyperlipidemia, atherosclerotic complications have been infrequently reported.
With diagnosis before serious harm occurs, prompt reversal of acidotic episodes, and appropriate long-term treatment, most children will be healthy. With exceptions and qualifications, adult health and life span may also be fairly good, although lack of effective treatment before the mid-1970s has limited our long-term information.

