
Epidural
Encyclopedia
- Did you mean Epidural hematomaEpidural hematomaEpidural or extradural hematoma is a type of traumatic brain injury in which a buildup of blood occurs between the dura mater and the skull. The dura mater also covers the spine, so epidural bleeds may also occur in the spinal column...
, a type of traumatic brain injury?
The term epidural is often short for epidural analgesia, a form of regional analgesia
Regional analgesia
Regional analgesia blocks passage of pain impulses through a nerve by depositing an analgesic drug close to the nerve trunk, cutting off sensory innervation to the region it supplies. The drug is normally injected at a site where the nerve is unprotected by bone.-See also:*Local...
involving injection of drugs through a catheter
Catheter
In medicine, a catheter is a tube that can be inserted into a body cavity, duct, or vessel. Catheters thereby allow drainage, administration of fluids or gases, or access by surgical instruments. The process of inserting a catheter is catheterization...
placed into the epidural space
Epidural space
In the spine, the epidural space is the outermost part of the spinal canal. It is the space within the canal lying outside the dura mater...
. The injection can cause both a loss of sensation (anaesthesia) and a loss of pain (analgesia), by blocking the transmission of signals through nerves in or near the spinal cord.
The epidural space
Epidural space
In the spine, the epidural space is the outermost part of the spinal canal. It is the space within the canal lying outside the dura mater...
is the space inside the bony spinal canal but outside the membrane called the dura mater
Dura mater
The dura mater , or dura, is the outermost of the three layers of the meninges surrounding the brain and spinal cord. It is derived from Mesoderm. The other two meningeal layers are the pia mater and the arachnoid mater. The dura surrounds the brain and the spinal cord and is responsible for...
(sometimes called the "dura"). In contact with the inner surface of the dura is another membrane called the arachnoid mater
Arachnoid mater
The arachnoid mater, literally from Latin "spider -like mother", is one of the three meninges, the membranes that cover the brain and spinal cord...
("arachnoid"). The arachnoid encompasses the cerebrospinal fluid
Cerebrospinal fluid
Cerebrospinal fluid , Liquor cerebrospinalis, is a clear, colorless, bodily fluid, that occupies the subarachnoid space and the ventricular system around and inside the brain and spinal cord...
that surrounds the spinal cord
Spinal cord
The spinal cord is a long, thin, tubular bundle of nervous tissue and support cells that extends from the brain . The brain and spinal cord together make up the central nervous system...
.
Difference from spinal anaesthesia
Spinal anaesthesiaSpinal anaesthesia
Spinal anaesthesia , also called spinal analgesia or sub-arachnoid block , is a form of regional anaesthesia involving injection of a local anaesthetic into the subarachnoid space, generally through a fine needle, usually 9 cm long...
is a technique whereby a local anaesthetic drug is injected into the cerebrospinal fluid
Cerebrospinal fluid
Cerebrospinal fluid , Liquor cerebrospinalis, is a clear, colorless, bodily fluid, that occupies the subarachnoid space and the ventricular system around and inside the brain and spinal cord...
. This technique has some similarity to epidural anaesthesia, and the two techniques may be easily confused with each other. Differences include:
- The involved space is larger for an epidural, and subsequently the injected dose is larger, being about 10-20 ml in epidural anesthesia compared to 1.5-3.5 ml in a spinal.
- In an epidural, an indwelling catheter may be placed that avails for additional injections later, while a spinal is usually one-shot only; though a continuous spinal can also be administered, especially in pain management (with morphineMorphineMorphine is a potent opiate analgesic medication and is considered to be the prototypical opioid. It was first isolated in 1804 by Friedrich Sertürner, first distributed by same in 1817, and first commercially sold by Merck in 1827, which at the time was a single small chemists' shop. It was more...
pumps). - The onset of analgesia is approximately 15–30 minutes in an epidural, while it is approximately 5 minutes in a spinal.
- An epidural usually doesn't cause significant neuromuscular block at the lower effective analgesicAnalgesicAn analgesic is any member of the group of drugs used to relieve pain . The word analgesic derives from Greek an- and algos ....
dosages, while a spinal more often does. - An epidural may be given at a thoracic or lumbar site, while a spinal must be injected below L2 to avoid piercing and consequently damaging the spinal cord.
- With epidural, it is possible to create segmental blocks as opposed to spinal where the block involves all segments below the highest level of anesthesia.
- The extension of the block with epidural anesthesia is highly dependent on the volume and rate of injection. The position of the patient has little to no impact on the level of the block whereas With spinal anesthesia, the density of the solution combined with the position of the patient influences the level of the block significantly.
Consequently, epidural is safer if a higher level of block is required.
Indications
Injecting medication into the epidural spaceEpidural space
In the spine, the epidural space is the outermost part of the spinal canal. It is the space within the canal lying outside the dura mater...
is primarily performed for analgesia. This may be performed using a number of different techniques and for a variety of reasons. Additionally, some of the side-effects of epidural analgesia may be beneficial in some circumstances (e.g., vasodilation
Vasodilation
Vasodilation refers to the widening of blood vessels resulting from relaxation of smooth muscle cells within the vessel walls, particularly in the large arteries, smaller arterioles and large veins. The process is essentially the opposite of vasoconstriction, or the narrowing of blood vessels. When...
may be beneficial if the patient has peripheral vascular disease). When a catheter
Catheter
In medicine, a catheter is a tube that can be inserted into a body cavity, duct, or vessel. Catheters thereby allow drainage, administration of fluids or gases, or access by surgical instruments. The process of inserting a catheter is catheterization...
is placed into the epidural space (see below) a continuous infusion can be maintained for several days, if needed. Epidural analgesia may be used:
- For analgesia alone, where surgery is not contemplated. An epidural for pain relief (e.g. in childbirthChildbirthChildbirth is the culmination of a human pregnancy or gestation period with the birth of one or more newborn infants from a woman's uterus...
) is unlikely to cause loss of muscle power, but is not usually sufficient for surgery. - As an adjunct to general anaesthesiaGeneral anaesthesiaGeneral anaesthesia is a state of unconsciousness and loss of protective reflexes resulting from the administration of one or more general anaesthetic agents...
. The anaesthetist may use epidural analgesia in addition to general anaesthesia. This may reduce the patient's requirement for opioidOpioidAn opioid is a psychoactive chemical that works by binding to opioid receptors, which are found principally in the central and peripheral nervous system and the gastrointestinal tract...
analgesics. This is suitable for a wide variety of surgery, for example gynaecological surgery (e.g. hysterectomyHysterectomyA hysterectomy is the surgical removal of the uterus, usually performed by a gynecologist. Hysterectomy may be total or partial...
), orthopaedic surgery (e.g. hip replacementHip replacementHip replacement is a surgical procedure in which the hip joint is replaced by a prosthetic implant. Hip replacement surgery can be performed as a total replacement or a hemi replacement. Such joint replacement orthopaedic surgery generally is conducted to relieve arthritis pain or fix severe...
), general surgery (e.g. laparotomyLaparotomyA laparotomy is a surgical procedure involving a large incision through the abdominal wall to gain access into the abdominal cavity. It is also known as coeliotomy.- Terminology :...
) and vascular surgery (e.g. open aortic aneurysmAortic aneurysmAn aortic aneurysm is a general term for any swelling of the aorta to greater than 1.5 times normal, usually representing an underlying weakness in the wall of the aorta at that location...
repair). See also caudal epidural, below. - As a sole technique for surgical anaesthesia. Some operations, most frequently Caesarean sectionCaesarean sectionA Caesarean section, is a surgical procedure in which one or more incisions are made through a mother's abdomen and uterus to deliver one or more babies, or, rarely, to remove a dead fetus...
, may be performed using an epidural anaesthetic as the sole technique. Typically the patient would remain awake during the operation. The dose required for anaesthesia is much higher than that required for analgesia. - For post-operative analgesia, after an operation where the epidural was used as either the sole anesthetic, or was used in combination with general anesthesia. Analgesics are given into the epidural space for a few days after surgery, provided a catheter has been inserted. Through the use of a patient-controlled epidural analgesia (PCEA) infusion pump, a patient has the ability to give an occasional extra dose of post-surgical pain medications administered through the epidural.
- For the treatment of back pain. Injection of analgesics and steroidSteroidA steroid is a type of organic compound that contains a characteristic arrangement of four cycloalkane rings that are joined to each other. Examples of steroids include the dietary fat cholesterol, the sex hormones estradiol and testosterone, and the anti-inflammatory drug dexamethasone.The core...
s into the epidural space may improve some forms of back pain. See below. - For the treatment of chronic pain or palliation of symptoms in terminal care, usually in the short- or medium-term.
The epidural space is more difficult and risky to access as one ascends the spine, so epidural techniques are most suitable for analgesia for the chest, abdomen, pelvis or legs. They are (usually) much less suitable for analgesia for the neck, or arms and are not possible for the head (since sensory innervation for the head arises directly from the brain via cranial nerves rather than from the spinal cord via the epidural space.)
Anatomy
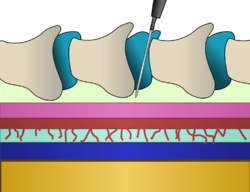
Pia mater
Pia mater often referred to as simply the pia, is the delicate innermost layer of the meninges, the membranes surrounding the brain and spinal cord. The word finds its roots in Latin, meaning literally "tender mother." The other two meningeal membranes are the dura mater and the arachnoid mater....
(blue). The arachnoid (red) exists superficial to the pia mater, and is attached to it by many trabeculae, giving it a spider-like appearance. This space (light blue) is filled with cerebrospinal fluid
Cerebrospinal fluid
Cerebrospinal fluid , Liquor cerebrospinalis, is a clear, colorless, bodily fluid, that occupies the subarachnoid space and the ventricular system around and inside the brain and spinal cord...
(CSF) and is called the subarachnoid space
Subarachnoid space
In the central nervous system, the subarachnoid cavity is the interval between the arachnoid membrane and pia mater....
. Superficial to the arachnoid is the dura mater
Dura mater
The dura mater , or dura, is the outermost of the three layers of the meninges surrounding the brain and spinal cord. It is derived from Mesoderm. The other two meningeal layers are the pia mater and the arachnoid mater. The dura surrounds the brain and the spinal cord and is responsible for...
(pink) and although they are unattached, they are kept firmly pressed against one another because of pressure exerted by the CSF. Superficial to the dura mater is a space (pale green), known as the epidural space, that exists between it and the internal surfaces of the vertebral bones and their supporting ligament
Ligament
In anatomy, the term ligament is used to denote any of three types of structures. Most commonly, it refers to fibrous tissue that connects bones to other bones and is also known as articular ligament, articular larua, fibrous ligament, or true ligament.Ligament can also refer to:* Peritoneal...
ous structures. This space is likewise pressed closed by surrounding tissue pressure, so it is called a 'potential' space. The vertebral bones (taupe) are attached to one another by the interspinous ligaments (teal). Insertion of an epidural involves threading a needle between the bones, through the ligaments and into the epidural potential space taking great care to avoid puncturing the layer immediately below containing CSF under pressure.
Technique of insertion
Epidural anaesthesia requires a high level of technical proficiency to avoid serious complications, and should always be performed by a trained anaesthetist or interventional radiologist under image guidance, using a strict aseptic techniqueAseptic technique
Aseptic technique refers to a procedure that is performed under sterile conditions. This includes medical and laboratory techniques, such as with microbiological cultures. It includes techniques like flame sterilization...
to reduce the risk of infection.
Position of the patient
The patient may be in the sitting or lateral position (lying on one side or prone). The sitting patient is asked to slouch and bend forward slightly from the waist to increase the curvature of the spine. The patient lying on the side is asked to draw the knees up to the chin for the same reason. If prone, a pillow is used to cause the back to arch.Insertion site
The anaesthetist palpates the patient's back and identifies a suitable anatomical gap between the bony spinous processes prior to the procedure. The level of the spine at which the catheter is best placed depends mainly on the site and type of an intended operation or the anatomical origin of pain. The iliac crests are commonly used for reference in order to locate the L4 vertebra, which is well below the termination of the spinal cord. Since innervation of the chest and abdomen travels under the ribs, the anaesthetist can palpate along the corresponding rib to determine placement of the catheter tip.Most commonly, the anaesthetist conducting an epidural places the catheter
Catheter
In medicine, a catheter is a tube that can be inserted into a body cavity, duct, or vessel. Catheters thereby allow drainage, administration of fluids or gases, or access by surgical instruments. The process of inserting a catheter is catheterization...
in the mid-lumbar
Lumbar
In tetrapod anatomy, lumbar is an adjective that means of or pertaining to the abdominal segment of the torso, between the diaphragm and the sacrum ...
, or lower back region of the spine
Vertebral column
In human anatomy, the vertebral column is a column usually consisting of 24 articulating vertebrae, and 9 fused vertebrae in the sacrum and the coccyx. It is situated in the dorsal aspect of the torso, separated by intervertebral discs...
, although occasionally a catheter is placed in the thoracic (chest) or cervical (neck) region. In adults, the spinal cord terminates around the level of the disc between L1 and L2 (in neonates it extends to L3 but can reach as low as L4), below which lies a bundle of nerves known as the cauda equina
Cauda equina
The cauda equina is a structure within the lower end of the spinal column of most vertebrates, that consists of nerve roots and rootlets from above...
("horse's tail"). Hence, lumbar epidurals carry a very low risk of injuring the spinal cord.
Locating the epidural space
The skin is infiltrated with local anaesthetic such as lidocaineLidocaine
Lidocaine , Xylocaine, or lignocaine is a common local anesthetic and antiarrhythmic drug. Lidocaine is used topically to relieve itching, burning and pain from skin inflammations, injected as a dental anesthetic or as a local anesthetic for minor surgery.- History :Lidocaine, the first amino...
over the identified space. The insertion point is usually in the midline, although other approaches, such as the paramedian approach, may occasionally be employed. In the paramedian approach, the needle tip passes along a shelf of vertebral bone called the lamina until just before reaching the ligamentun flavum and the epidural space. 'Walking' the needle tip off this lamina allows the clinician to be confident that they are close to the epidural space. This is particularly important in the thoracic spine, where the spinal cord is larger (than in the lumbar spine) and nearly fills the spinal canal increasing the risk of dural puncture and cord damage.
A particular type of needle known as a Tuohy needle
Tuohy needle
A Tuohy needle is a hollow hypodermic needle, very slightly curved at the end, suitable for inserting epidural catheters.The needle features an anti-coring curve at its tip, as shown in the picture above left.- Epidural needle :...
is almost invariably used. This needle was specially designed for locating the epidural space safely, and has several specific features for this purpose.
The Tuohy needle is inserted to the ligamentum flavum, is attached to a syringe in the peripheral end, and slowly advanced between two spinous process
Spinous process
The spinous process of a vertebra is directed backward and downward from the junction of the laminae , and serves for the attachment of muscles and ligaments. In animals without an erect stance, the process points upward and may slant forward or backward...
es. The loss of resistance to injection technique is used to identify the epidural space. This technique is to apply constant pressure on the piston of the syringe towards the barrel as if unfusing, and the loss of resistance is where it is be possible to inject through the syringe, so the piston can easily move into the barrel. This technique works because the ligamentum flavum is extremely dense, and injection into it is almost impossible. In the epidural space, on the other hand, there is negative or neutral pressure.
The syringe may contain air or saline. The principles are the same, but the specifics of the technique are different due to the greater compressibility of air with respect to saline.
Loss of resistance indicates a high likelihood that the tip of the needle has entered the epidural space. A sensation of "pop" or "click" may be felt as the needle breaches the ligamentum flavum just before entering the epidural space. A technique involving constant application of pressure to identify the epidural space whilst advancing the Tuohy needle was described as Dogliotti's principle
Dogliotti's principle
Dogliotti's principle is a principle in epidural anaesthesia first described by Professor Achille Mario Dogliotti in 1933. It is a method for the identification of the epidural space, a potential space...
in 1933. An innovative technique for teaching this sensation of 'loss of resistance' using a banana was described by Leighton in Anesthesiology 70:368-9; 1989 - "A greengrocer's model of the epidural space."
Traditionally anesthesiologist have used either air or saline
Saline (medicine)
In medicine, saline is a general term referring to a sterile solution of sodium chloride in water but is only sterile when it is to be placed intravenously, otherwise, a saline solution is a salt water solution...
for identifying the epidural space, depending on their personal preference. However, evidence is accumulating that saline may result in more rapid and satisfactory quality of analgesia.
In addition to the loss of resistance technique, realtime observation of the advancing needle is becoming more common. This may be done using a portable ultrasound
Ultrasound
Ultrasound is cyclic sound pressure with a frequency greater than the upper limit of human hearing. Ultrasound is thus not separated from "normal" sound based on differences in physical properties, only the fact that humans cannot hear it. Although this limit varies from person to person, it is...
scanner, or with fluoroscopy
Fluoroscopy
Fluoroscopy is an imaging technique commonly used by physicians to obtain real-time moving images of the internal structures of a patient through the use of a fluoroscope. In its simplest form, a fluoroscope consists of an X-ray source and fluorescent screen between which a patient is placed...
(moving X-ray pictures).
Feeding the catheter
After placement of the tip of the Tuohy needle into the epidural space the catheter is threaded through the needle. The needle is then withdrawn over the catheter. Generally the catheter is then withdrawn slightly so that 4–6 cm remains in the epidural space. The catheter has depth markings on it (see photo) so that the length of catheter in the epidural space can be estimated.The catheter is a fine plastic tube, down which anaesthetics may be given into the epidural space. Early catheters had a hole at the end ("end-hole catheters"), but were prone to blockage. More modern catheters ("side-hole catheters") have a blind end but three or more side-holes along the shaft near the tip. This not only disperses the anaesthetic more widely around the catheter, but lessens the likelihood of blockage.
The catheter is typically secured to the skin with adhesive tape or dressings to prevent it becoming dislodged.
In some unusual instances, it may not be required to insert a catheter into the epidural space, e.g. for steroid injections; see below. The anesthesiologist may inject medication into the epidural space through the needle, then remove the needle.
Anaesthetic drugs
A patient receiving an epidural for pain relief typically receives a combination of local anesthetics and opioidOpioid
An opioid is a psychoactive chemical that works by binding to opioid receptors, which are found principally in the central and peripheral nervous system and the gastrointestinal tract...
s. This combination works better than either type of drug used alone. Common local anesthetic
Local anesthetic
A local anesthetic is a drug that causes reversible local anesthesia, generally for the aim of having local analgesic effect, that is, inducing absence of pain sensation, although other local senses are often affected as well...
s include lidocaine
Lidocaine
Lidocaine , Xylocaine, or lignocaine is a common local anesthetic and antiarrhythmic drug. Lidocaine is used topically to relieve itching, burning and pain from skin inflammations, injected as a dental anesthetic or as a local anesthetic for minor surgery.- History :Lidocaine, the first amino...
, bupivacaine
Bupivacaine
Bupivacaine is a local anaesthetic drug belonging to the amino amide group. AstraZeneca commonly markets it under various trade names, including Marcain, Marcaine, Sensorcaine and Vivacaine.-Indications:...
, ropivacaine
Ropivacaine
Ropivacaine is a local anaesthetic drug belonging to the amino amide group. The name ropivacaine refers to both the racemate and the marketed S-enantiomer...
, and chloroprocaine
Chloroprocaine
Chloroprocaine is a local anesthetic given by injection during surgical procedures and labor and delivery. Chloroprocaine constricts blood vessels resulting in reduced blood loss; this is in contrast to other local anesthetics e.g. lidocaine, which do not do such...
. Common opioids include morphine
Morphine
Morphine is a potent opiate analgesic medication and is considered to be the prototypical opioid. It was first isolated in 1804 by Friedrich Sertürner, first distributed by same in 1817, and first commercially sold by Merck in 1827, which at the time was a single small chemists' shop. It was more...
, fentanyl, sufentanil
Sufentanil
Sufentanil is a powerful synthetic opioid analgesic drug, approximately 5 to 10 times more potent than its analog, fentanyl. Sufentanil is marketed for use by specialist centres under different trade names, such as Sufenta and Sufentil...
, and pethidine
Pethidine
Pethidine or meperidine Pethidine (INN) or meperidine (USAN) Pethidine (INN) or meperidine (USAN) (commonly referred to as Demerol but also referred to as: isonipecaine; lidol; pethanol; piridosal; Algil; Alodan; Centralgin; Dispadol; Dolantin; Mialgin (in Indonesia); Petidin Dolargan (in Poland);...
(known as meperidine in the U.S.). These are injected in relatively small doses.
Occasionally other agents may be used, such as clonidine
Clonidine
Clonidine is a sympatholytic medication used to treat medical conditions, such as high blood pressure, some pain conditions, ADHD and anxiety/panic disorder...
or ketamine
Ketamine
Ketamine is a drug used in human and veterinary medicine. Its hydrochloride salt is sold as Ketanest, Ketaset, and Ketalar. Pharmacologically, ketamine is classified as an NMDA receptor antagonist...
.
Bolus or infusion?

Bolus (medicine)
In medicine, a bolus is the administration of a medication, drug or other compound that is given to raise its concentration in blood to an effective level...
). This will eventually wear off. Thereafter, the anaesthetist may repeat the bolus provided the catheter remains undisturbed.
For a prolonged effect, a continuous infusion of drugs may be employed. A common solution for epidural infusion in childbirth
Childbirth
Childbirth is the culmination of a human pregnancy or gestation period with the birth of one or more newborn infants from a woman's uterus...
or for post-operative analgesia is 0.2% ropivacaine
Ropivacaine
Ropivacaine is a local anaesthetic drug belonging to the amino amide group. The name ropivacaine refers to both the racemate and the marketed S-enantiomer...
or 0.125% bupivacaine
Bupivacaine
Bupivacaine is a local anaesthetic drug belonging to the amino amide group. AstraZeneca commonly markets it under various trade names, including Marcain, Marcaine, Sensorcaine and Vivacaine.-Indications:...
, with 2 μg/mL of fentanyl added. This solution is infused at a rate between 4 and 14 mL/hour, following a loading dose to initiate the nerve block
Nerve block
Regional nerve blockade, or more commonly nerve block, is a general term used to refer to the injection of local anesthetic onto or near nerves for temporary control of pain. It can also be used as a diagnostic tool to identify specific nerves as pain generators...
.
There is some evidence that an automated intermittent bolus technique provides better analgesia than a continuous infusion technique, though the total doses are identical.
Block height and intensity
Typically, the effects of the epidural are noted below a specific level on the body (dermatomeDermatome
Dermatome may refer to:*Dermatome , a surgical instrument used to produce thin slices of skin*Dermatome , an area of skin that is supplied by a single pair of dorsal roots*Dermatome...
). This level (the "block height") is chosen by the anaesthetist. The level is usually 3-4 dermatomes higher than the point of insertion. A very high insertion level may result in sparing of very low dermatomes. For example, a thoracic epidural may be performed for upper abdominal surgery, but may not have any effect on the perineum
Perineum
In human anatomy, the perineum is a region of the body including the perineal body and surrounding structures...
(area around the genitals) or bladder. Nonetheless, giving very large volumes into the epidural space may spread the block both higher and lower.
The intensity of the block is determined by the concentration of local anaesthetic drugs used. For example, 15 ml 0.1% bupivacaine may provide good analgesia for a woman in labour, but would likely be insufficient for surgery. Conversely, 15 ml of 0.5% bupivacaine would provide a more intense block, likely sufficient for surgery. Since the volume used in each case is the same, the spread of drug, and hence the block height, is likely to be similar.
Removing the catheter
The catheter is usually removed when the patient is able to take oral pain medications. Catheters can safely remain in place for several days with little risk of bacterial infection, particularly if the skin is prepared with a chlorhexidine solution. Subcutaneously tunneled epidural catheters may be left in place for longer periods, with a low risk of infection or other complications. Before removing the catheter, the anticoagulation status of the patient must be checked. If the patient is on anticoagulation therapy, it must be stopped for at least 12 hours before the catheter is removed. After removing the catheter, anticoagulation may be resumed after a wait of 2 hours.Combined spinal-epidurals
For some procedures, the anaesthetist may choose to combine the rapid onset and reliable, dense block of a spinal anaestheticSpinal anaesthesia
Spinal anaesthesia , also called spinal analgesia or sub-arachnoid block , is a form of regional anaesthesia involving injection of a local anaesthetic into the subarachnoid space, generally through a fine needle, usually 9 cm long...
with the post-operative analgesic effects of an epidural. This is called combined spinal and epidural anaesthesia
Combined spinal and epidural anaesthesia
Combined spinal and epidural anaesthesia is a regional anaesthetic technique, which combines the benefits of both spinal anaesthesia and epidural anaesthesia and analgesia. The spinal component gives a rapid onset of a predictable block...
(CSE).
The anaesthetist may insert the spinal anaesthetic at one level, and the epidural at an adjacent level. Alternatively, after locating the epidural space with the Tuohy needle, a spinal needle may be inserted through the Tuohy needle into the subarachnoid space. The spinal dose is then given, the spinal needle withdrawn, and the epidural catheter inserted as normal. This method, known as the "needle-through-needle" technique, may be associated with a slightly higher risk of placing the catheter into the subarachnoid space.
Caudal epidurals
The epidural space may be entered through the sacrococcygeal membraneSacrococcygeal membrane
The sacrococcygeal membrane is a tough fibrous membrane about 10mm long which extends from the inferior tip of the sacrum to the body of the coccyx in humans...
, using a 22g catheter-over-needle or regular 21G needle. Injecting a volume of 1 cc/kg of local anaesthetic here provides good analgesia of the perineum
Perineum
In human anatomy, the perineum is a region of the body including the perineal body and surrounding structures...
and groin areas. This is typically a single-injection technique and a catheter is not normally placed. This is known as a caudal epidural or "caudal".
The caudal epidural is an effective and safe analgesic technique in children undergoing groin, pelvic or lower extremity surgery. It is usually combined with general anaesthesia since children cannot tolerate the injection awake.
Epidural steroid injections
An epidural steroid injectionEpidural Steroid Injection
Epidural Steroid Injection is a technique for relieving pain from spinal stenosis and spinal disc herniation. Using a needle, relatively small amounts of corticosteroids together with a local anesthetic are injected into the epidural space around the spinal cord and spinal nerves...
injection may be used to help reduce the pain and inflammation caused by herniated disc, degenerative disc disease
Degenerative disc disease
Degeneration of the intervertebral disc, often called "degenerative disc disease" of the spine, is a condition that can be painful and can greatly affect the quality of one's life...
, or spinal stenosis
Spinal stenosis
Lumbar spinal stenosis is a medical condition in which the spinal canal narrows and compresses the spinal cord and nerves at the level of the lumbar vertebra. This is usually due to the common occurrence of spinal degeneration that occurs with aging. It can also sometimes be caused by spinal disc...
.
Benefits of epidural analgesia after surgery
Epidural analgesia has been demonstrated to have several benefits after surgery. These include:- Effective analgesia without the need for systemic opioids.
- The incidence of postoperative respiratory problems and chest infections is reduced.
- The incidence of postoperative myocardial infarctionMyocardial infarctionMyocardial infarction or acute myocardial infarction , commonly known as a heart attack, results from the interruption of blood supply to a part of the heart, causing heart cells to die...
("heart attack") is reduced. - The stress response to surgery is reduced.
- Motility of the intestines is improved by blockade of the sympathetic nervous system.
- Use of epidural analgesia during surgery reduces blood transfusionBlood transfusionBlood transfusion is the process of receiving blood products into one's circulation intravenously. Transfusions are used in a variety of medical conditions to replace lost components of the blood...
requirements.
Despite these benefits, no survival benefit has been proven for high-risk patients.
Side effects
In addition to blocking the nerves which carry pain, local anaesthetic drugs in the epidural space will block other types of nerves as well, in a dose-dependent manner. Depending on the drug and dose used, the effects may last only a few minutes or up to several hours. Epidural typically involves using the opiates fentanyl or sufentanil, with bupivacaine, Fentanyl is a powerful opioid with a potency 80 times that of morphine and side effects common to the opiate class. Sufentanil is another opiate, 5 to 10Xs more potent than Fentanyl. Bupivacaine is markedly toxic, causing excitation: nervousness, tingling around the mouth, tinnitus, tremor, dizziness, blurred vision, or seizures, followed by depression: drowsiness, loss of consciousness, respiratory depression and apnea. Bupivacaine has caused several deaths by cardiac arrest when epidural anesthetic has been accidentally inserted into vein instead of epidural space in the spine. Epidural correctly administered results in three main effects:- Loss of other modalities of sensation (including touch, and proprioceptionProprioceptionProprioception , from Latin proprius, meaning "one's own" and perception, is the sense of the relative position of neighbouring parts of the body and strength of effort being employed in movement...
) - Loss of muscle power (hence, a risk of falling)
- Loss of function of the sympathetic nervous systemSympathetic nervous systemThe sympathetic nervous system is one of the three parts of the autonomic nervous system, along with the enteric and parasympathetic systems. Its general action is to mobilize the body's nervous system fight-or-flight response...
, which controls blood pressureBlood pressureBlood pressure is the pressure exerted by circulating blood upon the walls of blood vessels, and is one of the principal vital signs. When used without further specification, "blood pressure" usually refers to the arterial pressure of the systemic circulation. During each heartbeat, BP varies...
Pain nerves are most sensitive to the effects of the epidural. This means that a good epidural can provide analgesia without affecting muscle power or other types of sensation. The larger the dose used, the more likely it is that the side-effects will be problematic.
For example, a laboring woman may have a continuous epidural during labor that in 85% of cases provides good analgesia without impairing her ability to move around in bed. If she requires a Caesarean section, she is given a larger dose of epidural bupivacaine
Bupivacaine
Bupivacaine is a local anaesthetic drug belonging to the amino amide group. AstraZeneca commonly markets it under various trade names, including Marcain, Marcaine, Sensorcaine and Vivacaine.-Indications:...
. After a few minutes, she can no longer move her legs, or feel her abdomen. If her blood pressure drops below 80/50 she is given an intravenous bolus of ephedrine or phenylephrine
Phenylephrine
Phenylephrine is a selective α1-adrenergic receptor agonist used primarily as a decongestant, as an agent to dilate the pupil, and to increase blood pressure...
infusion to compensate. During the operation, she feels no pain.
Very large doses of epidural anaesthetic can cause paralysis of the intercostal
Intercostal
Intercostal means "between the ribs". It can refer to:* Intercostal muscle* Highest intercostal vein* Intercostal arteries* Intercostal space...
muscles and diaphragm
Thoracic diaphragm
In the anatomy of mammals, the thoracic diaphragm, or simply the diaphragm , is a sheet of internal skeletal muscle that extends across the bottom of the rib cage. The diaphragm separates the thoracic cavity from the abdominal cavity and performs an important function in respiration...
(which are responsible for breathing), and loss of sympathetic function to the heart itself, causing a profound drop in heart rate and blood pressure. This requires emergency treatment, and in severe cases may require airway support. This happens because the epidural is blocking the heart's sympathetic nerves, as well as the phrenic nerve
Phrenic nerve
The phrenic nerve originates mainly from the 4th cervical nerve, but also receives contributions from the 5th and 3rd cervical nerves in humans....
s, which supply the diaphragm.
It is considered safe practice for all patients with epidurals to be confined to bed to prevent the risk of falls.
The sensation of needing to urinate is diminished, which often requires the placement of a urinary catheter
Urinary catheterization
In urinary catheterization , a latex, polyurethane or silicone tube known as a urinary catheter is inserted into a patient's bladder via his or her urethra. Catheterization allows the patient's urine to drain freely from the bladder for collection. It may be used to inject liquids used for...
for the duration of the epidural
Opioid drugs in the epidural space are relatively safe (as well as effective). However, very large doses may cause troublesome itch, and rarely, delayed respiratory depression.
Relative contraindications
There are circumstances where the risks of an epidural are higher than normal. These circumstances include:- Anatomical abnormalities, such as spina bifidaSpina bifidaSpina bifida is a developmental congenital disorder caused by the incomplete closing of the embryonic neural tube. Some vertebrae overlying the spinal cord are not fully formed and remain unfused and open. If the opening is large enough, this allows a portion of the spinal cord to protrude through...
or scoliosisScoliosisScoliosis is a medical condition in which a person's spine is curved from side to side. Although it is a complex three-dimensional deformity, on an X-ray, viewed from the rear, the spine of an individual with scoliosis may look more like an "S" or a "C" than a straight line... - Previous spinal surgery (where scar tissue may hamper the spread of medication, or may cause an acquired tethered spinal cord)
- Certain problems of the central nervous system, including multiple sclerosisMultiple sclerosisMultiple sclerosis is an inflammatory disease in which the fatty myelin sheaths around the axons of the brain and spinal cord are damaged, leading to demyelination and scarring as well as a broad spectrum of signs and symptoms...
or syringomyeliaSyringomyeliaSyringomyelia is a generic term referring to a disorder in which a cyst or cavity forms within the spinal cord. This cyst, called a syrinx, can expand and elongate over time, destroying the spinal cord. The damage may result in pain, paralysis, weakness, and stiffness in the back, shoulders, and... - Certain heart-valve problems (such as aortic stenosis, where the vasodilation induced by the anesthetic may impair blood supply to the thickened heart muscle.)
Absolute contraindications
Circumstances in which epidurals should not be used:- Lack of consent
- Bleeding disorder (coagulopathyCoagulopathyCoagulopathy is a condition in which the blood’s ability to clot is impaired. This condition can cause prolonged or excessive bleeding, which may occur spontaneously or following an injury or medical and dental procedures.The normal clotting process depends on the interplay of various proteins in...
) or anticoagulant medication (e.g. warfarinWarfarinWarfarin is an anticoagulant. It is most likely to be the drug popularly referred to as a "blood thinner," yet this is a misnomer, since it does not affect the thickness or viscosity of blood...
) - risk of spinal cord-compressing hematoma - Infection near the point of intended insertion
- Infection in the bloodstream which may "seed" via the catheter into the (otherwise relatively impervious) central nervous system
- Uncorrected hypovolemia (low circulating blood volume)
- Allergy to the anaesthetic
Complications and questions about epidural use
These include:- No pain relief, also called "block failure," occurs in about 5% of patients, while another 15% experience partial relief, sometimes colloquially called a "patchy blockade." If pain relief is inadequate, another epidural may be attempted. Note that regardless of the effect of the epidural on pain relief, once an epidural is administered, many hospitals do not allow patients to get out of bed. A fully effective epidural would prevent a patient from walking at all, however, so this is only a matter of interest in failed attempts. Modern epidural procedures can be done in some hospitals without compromising the mobility of the patient. This is generally referred to as a "walking epidural" and is actually a combination of a traditional epidural block with a spinal injection. Walking is generally encouraged postoperatively in ERAS protocol, once the effect of the epidural has diminished to the point where the patient has enough muscle strength to remain upright.
- The following factors are associated with no pain relief, or block failure with epidurals:
- ObesityObesityObesity is a medical condition in which excess body fat has accumulated to the extent that it may have an adverse effect on health, leading to reduced life expectancy and/or increased health problems...
- Multiparity
- History of a previous failure of epidural anesthesia
- History of regular opiateOpiateIn medicine, the term opiate describes any of the narcotic opioid alkaloids found as natural products in the opium poppy plant.-Overview:Opiates are so named because they are constituents or derivatives of constituents found in opium, which is processed from the latex sap of the opium poppy,...
use - Cervical dilationCervical dilationCervical dilation is the opening of the cervix, the entrance to the uterus, during childbirth, miscarriage, induced abortion, or gynecological surgery...
of more than 7 cm at insertion - The use of air to find the epidural space while inserting the epidural instead of alternatives like N2O, saline or lidocaine
- Obesity
- The following factors are associated with no pain relief, or block failure with epidurals:
- Accidental dural puncture with headache (common, about 1 in 100 insertions). The epidural space in the adult lumbar spine is only 3-5mm deep, which means it is comparatively easy to cross it and accidentally puncture the dura (and arachnoid) with the needle. This may cause cerebrospinal fluid (CSF) to leak out into the epidural space, which may in turn cause a post dural puncture headache (PDPH). This can be severe and last several days, and in some rare cases weeks or months. It is caused by a reduction in CSF pressure and is characterised by postural exacerbation when the patient raises their head above the lying position. If severe it may be successfully treated with an epidural blood patchEpidural blood patchAn epidural blood patch is a surgical procedure which uses autologous blood in order to close one or many holes in the dura mater of the spinal cord, usually as a result of a previous lumbar puncture. The procedure can be used to relieve post dural puncture headaches caused by lumbar puncture...
(a small amount of the patient's own blood given into the epidural space via another epidural needle which clots and seals the leak). Most cases resolve spontaneously with time. A change in headache pattern (e.g., headache worse when you lie down) should alert the physician to the possibility of development of rare but dangerous complications, such as subdural hematomaSubdural hematomaA subdural hematoma or subdural haematoma , also known as a subdural haemorrhage , is a type of haematoma, a form of traumatic brain injury. Blood gathers within the outermost meningeal layer, between the dura mater, which adheres to the skull, and the arachnoid mater, which envelops the brain...
or cerebral venous thrombosis.
- Delayed onset of breastfeeding and shorter duration of breastfeeding: In a study looking at breastfeeding 2 days after epidural anesthesia, epidural analgesia in combination with oxytocin infusion caused women to have significantly lower oxytocin and prolactin levels in response to the baby breastfeeding on day 2 postpartum, which means less milk is produced. Most women with epidurals end up with pitocin augmentation because the epidural slows down the labor.
- Bloody tap (about 1 in 30-50). It is easy to injure an epidural vein with the needle. In patients who have normal blood clotting, it is extremely rare (e.g. 1 in 100,000) for problems to develop. However, in a patient who has a coagulopathyCoagulopathyCoagulopathy is a condition in which the blood’s ability to clot is impaired. This condition can cause prolonged or excessive bleeding, which may occur spontaneously or following an injury or medical and dental procedures.The normal clotting process depends on the interplay of various proteins in...
, the patient may be at risk of epidural hematomaEpidural hematomaEpidural or extradural hematoma is a type of traumatic brain injury in which a buildup of blood occurs between the dura mater and the skull. The dura mater also covers the spine, so epidural bleeds may also occur in the spinal column...
. If blood comes back down the needle, the anesthesiologist will normally place the epidural at another level.
- Catheter misplaced into a vein (uncommon, less than 1 in 300). Occasionally the catheter may be misplaced into an epidural vein, which results in all the anaesthetic being injected intravenously, where it can cause seizures or cardiac arrest in large doses (about 1 in 10,000 insertions). This also results in block failure.
- High block, as described above (uncommon, less than 1 in 500).
- Catheter misplaced into the subarachnoid space (rare, less than 1 in 1000). If the catheter is accidentally misplaced into the subarachnoid space (e.g. after an unrecognised accidental dural puncture), normally cerebrospinal fluid can be freely aspirated from the catheter (which would usually prompt the anaesthetist to withdraw the catheter and resite it elsewhere). If, however, this is not recognised, large doses of anaesthetic may be delivered directly into the cerebrospinal fluid. This may result in a high block, or, more rarely, a total spinal, where anaesthetic is delivered directly to the brainstem, causing unconsciousness and sometimes seizures.
- Neurological injury lasting less than 1 year (rare, about 1 in 6,700).
- Epidural abscess formation (very rare, about 1 in 145,000). Infection risk increases with the duration catheters are left in place, although infection was still uncommon after an average of 3 to 5 days' duration.http://www.ncbi.nlm.nih.gov/pubmed/8087910http://www.ncbi.nlm.nih.gov/pubmed/7574052
- Epidural haematoma formation (very rare, about 1 in 168,000).
- Neurological injury lasting longer than 1 year (extremely rare, about 1 in 240,000).
- ParaplegiaParaplegiaParaplegia is an impairment in motor or sensory function of the lower extremities. The word comes from Ionic Greek: παραπληγίη "half-striking". It is usually the result of spinal cord injury or a congenital condition such as spina bifida that affects the neural elements of the spinal canal...
(1 in 250,000). - ArachnoiditisArachnoiditisArachnoiditis is a neuropathic disease caused by the inflammation of the arachnoid, one of the membranes that surround and protect the nerves of the central nervous system, including the brain and spinal cord...
(extremely rare, fewer than 1000 cases in the past 50 years) - DeathDeathDeath is the permanent termination of the biological functions that sustain a living organism. Phenomena which commonly bring about death include old age, predation, malnutrition, disease, and accidents or trauma resulting in terminal injury....
(extremely rare, less than 1 in 100,000).
The figures above relate to epidurals in healthy individuals.
There is no evidence to support the concern that epidural analgesia increases the risk of anastomotic
Anastomosis
An anastomosis is the reconnection of two streams that previously branched out, such as blood vessels or leaf veins. The term is used in medicine, biology, mycology and geology....
breakdown following bowel surgery.
Controversial Claims:
- The claim that "epidurals significantly slow labor" is considered controversial. This claim is explored in greater detail in further sections of the topic. The following are a few plausible hypotheses for this phenomenon:
- The release of oxytocin, which stimulates the uterine contractions of labor that are needed to move the child out through the birth canal, may be decreased with epidurals due to factors involving the reduction of stress, such as:
- While an epidural is primarily used to alleviate pain during labor, it may also alleviate some of the stress, thereby diminishing the release of epinephrineEpinephrineEpinephrine is a hormone and a neurotransmitter. It increases heart rate, constricts blood vessels, dilates air passages and participates in the fight-or-flight response of the sympathetic nervous system. In chemical terms, adrenaline is one of a group of monoamines called the catecholamines...
(a natural product of the adrenal glands located atop the kidneys; generally released in association with high levels of stress).- Diminished release of epinephrine slows the release of oxytocin, because the adrenal glands are controlled by the hypothalamus rather than by hormones.
- Diminished blood pressure, accommodated by both decreased stress and less adrenal release, may decrease the release of oxytocin as a natural mechanism to avoid hypotension. It may also affect the heart-rate of the fetus.
- While an epidural is primarily used to alleviate pain during labor, it may also alleviate some of the stress, thereby diminishing the release of epinephrine
- The release of oxytocin, which stimulates the uterine contractions of labor that are needed to move the child out through the birth canal, may be decreased with epidurals due to factors involving the reduction of stress, such as:
- Still plausible (though less studied without a documented reproduction in a laboratory setting) are the effects of the reclined position of the woman on the fetus, both immediately prior to and during delivery.
- These hypotheses generally posit an interaction with the force of gravity on fetal position and movement, as demonstrated by the following examples:
- Transverse or posterior fetal positioning may become more likely as a result of the shift in orientation to gravitational force.
- Diminished gravitational assistance is present in building pressure for commencing delivery and for progressing the fetus along the birth canal.
- It is important to note that the orientation of the fetus can be established by ultrasonic stenography prior to, during, and after the administration of an epidural block. This would seem a fine experiment for testing the first hypothesis. It should also be noted that the majority of fetal movement through the birth canal is accomplished by cervical contractions, and so the role of gravity and its force relative to the position of the woman in labor (on delivery, not development) is difficult to establish.
- These hypotheses generally posit an interaction with the force of gravity on fetal position and movement, as demonstrated by the following examples:
- There has been a good deal of concern, based on older observational studies, that women who have epidural analgesia during labor are more likely to require a cesarean delivery. However, the preponderance of evidence now supports the conclusion that the use of epidural analgesia during labor does not have a significant effect on rates of cesarean delivery. A Cochrane review of 20 trials involving a total of 6534 women estimated that the relative risk of cesarean delivery with epidural analgesia as compared with other methods or with no analgesia was 1.07 (95% confidence interval, 0.93 to 1.23).31 Epidural analgesia does increase the duration of the second stage of labor by 15 to 30 minutes and may increase the rate of instrument-assisted vaginal deliveries as well as that of oxytocin administration. Clinicians and patients have also been concerned about whether the use of epidural analgesia in early labor increases the risk of cesarean delivery. Three randomized, controlled trials showed that early initiation of epidural analgesia (cervical dilatation, <4 cm) does not increase the rate of cesarean delivery among women with spontaneous or induced labor, as compared with early initiation of analgesia with parenteral opioids.
Safety and efficacy
Epidural analgesia is a relatively safe method of relieving pain in labor. It provides rapid pain relief in most cases. It is more effective than nitrous oxideNitrous oxide
Nitrous oxide, commonly known as laughing gas or sweet air, is a chemical compound with the formula . It is an oxide of nitrogen. At room temperature, it is a colorless non-flammable gas, with a slightly sweet odor and taste. It is used in surgery and dentistry for its anesthetic and analgesic...
, opioids, TENS, and other common modalities of analgesia in childbirth. Epidural clonidine has been studied extensively for management of analgesia during labor.
Prolonged labour and risk of instrumental delivery
Epidural analgesia is associated with longer labor. Some researchers claim that it is correlated with an increased chance of operational intervention. The clinical research data on this topic is conflicting. For example, a study in Australia (Roberts, Tracy, Peat, 2000) concluded that having an epidural reduced the woman's chances of having a vaginal birth, without further interventions (such as episiotomyEpisiotomy
An episiotomy , also known as perineotomy, is a surgically planned incision on the perineum and the posterior vaginal wall during second stage of labor. The incision, which can be midline or at an angle from the posterior end of the vulva, is performed under local anaesthetic , and is sutured...
, forceps
Forceps
Forceps or forcipes are a handheld, hinged instrument used for grasping and holding objects. Forceps are used when fingers are too large to grasp small objects or when many objects need to be held at one time while the hands are used to perform a task. The term 'forceps' is used almost exclusively...
, ventouse
Ventouse
Ventouse is a vacuum device used to assist the delivery of a baby when the second stage of labour has not progressed adequately. It is an alternative to a forceps delivery and caesarean section. It cannot be used when the baby is in the breech position or for premature births. This technique is...
or caesarean section
Caesarean section
A Caesarean section, is a surgical procedure in which one or more incisions are made through a mother's abdomen and uterus to deliver one or more babies, or, rarely, to remove a dead fetus...
) from 71.4% to 37.8%. Conversely, a 2001 study by researchers at the National Institute of Child Health and Human Development
National Institute of Child Health and Human Development
The Eunice Kennedy Shriver National Institute of Child Health and Human Development , created by Congress in 1962, supports and conducts research on topics related to the health of children, adults, families, and populations...
and a 2002 study by researchers at Cornell University
Cornell University
Cornell University is an Ivy League university located in Ithaca, New York, United States. It is a private land-grant university, receiving annual funding from the State of New York for certain educational missions...
and the University of Ontario demonstrated that epidurals do not increase the likelihood of a caesarean section, however the later one confirmed higher frequency of instrumental delivery and fewer and both of them confirmed prolongation of second stage. In 2005, a meta-analysis of 21 studies also showed that epidurals do not increase the likelihood of caesarean section, but they do increase the chance of a forceps or ventouse
Ventouse
Ventouse is a vacuum device used to assist the delivery of a baby when the second stage of labour has not progressed adequately. It is an alternative to a forceps delivery and caesarean section. It cannot be used when the baby is in the breech position or for premature births. This technique is...
delivery by 40% (Anim-Somuah, Cochrane Review, 2005). However, the 2000 and 2005 Cochrane Review Meta-Analyses were both driven by a single study by Sharma and colleagues which was based upon a hospital where the caesarean section
Caesarean section
A Caesarean section, is a surgical procedure in which one or more incisions are made through a mother's abdomen and uterus to deliver one or more babies, or, rarely, to remove a dead fetus...
rate was roughly 1/3 of the national average. This facility's physicians presumably prefer vaginal deliveries and avoid caesarean section
Caesarean section
A Caesarean section, is a surgical procedure in which one or more incisions are made through a mother's abdomen and uterus to deliver one or more babies, or, rarely, to remove a dead fetus...
s. Because of how low the caesarean section
Caesarean section
A Caesarean section, is a surgical procedure in which one or more incisions are made through a mother's abdomen and uterus to deliver one or more babies, or, rarely, to remove a dead fetus...
rates were in this facility, the data could not have shown a difference in caesarean rates between epidural and other methods of anagelsia. In fact, when the study is adjusted for this and other statistical issues, the rate of caesarean section
Caesarean section
A Caesarean section, is a surgical procedure in which one or more incisions are made through a mother's abdomen and uterus to deliver one or more babies, or, rarely, to remove a dead fetus...
is 259% (95% CI 129% to 523%) with epidural versus other analgesics. The COMET Study, published in The Lancet in 2001 (vol358, No9275 p19-23) showed that a combined spinal epidural in labor may speed up the labor process by a few minutes, although those women receiving an epidural had a caesarean rate of 28% and only 35% had a normal birth without instrument assisted delivery.
These differing outcomes may be explained by data that demonstrates that the likelihood of increased intervention is directly related to the quality of the institution or practitioner providing the care: epidurals administered at top-rated institutions do not generally result in a clinically significant increase in caesarean rates, whereas the risk of caesarean delivery at poorly ranked facilities seems to increase with the use of epidural
Effects on the baby
One study concluded that women whose epidurals contain the drug fentanyl were less likely to fully breastfeed their infant in the few days after birth and more likely to stop breastfeeding in the first 24 weeks. However, this study has been criticised for several reasons, one of which is that the original patient records were not examined in this study, and so many of the epidurals were assumed to contain fentanyl when almost certainly they would not have. In addition, all patients who used epidurals in labor had also used systemic pethidine, which would be much more likely to be the cause of any effect on breastfeeding due to the higher amounts of medication used via that route. If that were the case, then early epidurals which avoided the need for pethidine may actually improve breastfeeding outcomes, not worsen them.Historical notes
In 1901, the use of anaesthesics via the epidural space was first reported, mostly for the treatment of urological diseases but not for surgical procedures. Several techniques were developed in the following years, but never became popular for surgical purposes: most institutions made the transition from a slight sedation to twilight sleep to heavy sedation to general anaesthesia. Caesarean sectionCaesarean section
A Caesarean section, is a surgical procedure in which one or more incisions are made through a mother's abdomen and uterus to deliver one or more babies, or, rarely, to remove a dead fetus...
s under general anesthesia were used only as an emergency measure. In 1912, German physicians found that the injection of an anesthetic, at the base of the spinal cord, would prevent pain impulses from reaching the brain. For expectant mothers, the injection "only reduced the pangs of childbirth; it did not eliminate them," wrote Dr. Morris Fishbein in the March 1943 issue of Hygeia, and a single nerve blocking injection was used only toward the end of labor.
In the 1921, Spanish military surgeon Fidel Pagés
Fidel Pagés
Fidel Pagés Miravé was a Spanish military surgeon, known for developing the technique of epidural anesthesia....
developed the modern technique of lumbar epidural anaesthesia, which was popularised in the 1930s by Italian surgery professor Achile Mario Dogliotti.
Dr. Robert A. Hingson, Dr. Waldo B. Edwards, and Dr. James L. Southworth working at the United States Marine Hospital at Stapleton, on Staten Island, New York, developed the technique of continuous caudal anesthesia. Drs. Hingson and Southworth combined the concepts of caudal analgesia and the spinal injection in an operation to strip the varicose veins of a Scottish merchant seaman. The surgeons experimented with a continuous infusion of the local anesthetic, rather than removing the needle after the injection, to originate "continuous caudal analgesia". Dr. Hingson then collaborated with Dr. Edwards, the chief obstetrician at the Marine Hospital, to study the use of this technique in childbirth. The two studied the caudal region to determine where a needle could be safely placed to deliver anesthesia to the spinal nerves without placing the drugs into the spinal fluid.
Testing on a human being did not occur until January 6, 1942, when the wife of a Coast Guard
Coast guard
A coast guard or coastguard is a national organization responsible for various services at sea. However the term implies widely different responsibilities in different countries, from being a heavily armed military force with customs and security duties to being a volunteer organization tasked with...
sman was brought into the Marine Hospital for a delivery. Because the woman suffered from rheumatic heart disease
Heart disease
Heart disease, cardiac disease or cardiopathy is an umbrella term for a variety of diseases affecting the heart. , it is the leading cause of death in the United States, England, Canada and Wales, accounting for 25.4% of the total deaths in the United States.-Types:-Coronary heart disease:Coronary...
, general anesthesia could not be safely used for an emergency Caesarean section
Caesarean section
A Caesarean section, is a surgical procedure in which one or more incisions are made through a mother's abdomen and uterus to deliver one or more babies, or, rarely, to remove a dead fetus...
, and it was believed that she would not survive the stress of labor. With the use of continuous local anesthesia, the woman and her baby survived. According to Dr. Fishbein's article in Hygeia, a total of 589 women in more than twenty participating hospitals gave birth relatively painlessly in 1942.
The results were published in the January 23, 1943, issue of the Journal of the American Medical Association
Journal of the American Medical Association
The Journal of the American Medical Association is a weekly, peer-reviewed, medical journal, published by the American Medical Association. Beginning in July 2011, the editor in chief will be Howard C. Bauchner, vice chairman of pediatrics at Boston University’s School of Medicine, replacing ...
.
Further reading
- Boqing Chen and Patrick M. Foye, UMDNJ: New Jersey Medical School, Epidural Steroid Injections: Non-surgical Treatment of Spine Pain, eMedicine: Physical Medicine and Rehabilitation (PM&R), August 2005. Also available online.
External links
- Epidurals for pain relief in labour Comprehensive information with women's stories - informedhealthonline.org, Accessed July 2, 2009.
- Epidural and nerve root injections pain treatment explained
- What Is An Epidural Headache? - Epidural Headaches Explained

