Interventional radiology
Encyclopedia
Interventional radiology (abbreviated IR or sometimes VIR for Vascular and Interventional Radiology, also known as Image-Guided Surgery, Surgical Radiology, and "Pinhole" Surgery) is a specialty of radiology
, in which image-guided procedures are used to diagnose and treat a multitude of diseases across all body systems. Interventional radiologists are board-certified physicians who specialize in these minimally invasive, targeted treatments. They offer the most in-depth knowledge of the least invasive treatments available coupled with diagnostic and clinical experience across all specialties. They use X-rays, CT, ultrasound, MRI and other imaging modalities to advance a catheter or probe in the body to treat at the source of the disease non-surgically. As the inventors of angioplasty and the catheter-delivered stent, which were first used in the legs to treat peripheral arterial disease, interventional radiologists are the pioneers of minimally invasive modern medicine.
Today many conditions that once required surgery can be treated nonsurgically by interventional radiologists. Some of these procedures are done for purely diagnostic purposes (e.g., angiogram
), while others are done for treatment purposes (e.g., angioplasty
). Interventional radiology treatments offer less risk, pain, and recovery time compared to open surgery.
The basic concept behind interventional radiology is to diagnose or treat pathology using the least invasive technique possible. Images are used to direct interventional procedures, which are usually done with needles and narrow tubes called catheter
s. The images provide road maps that allow the interventional radiologist to guide these instruments through the body to the areas containing disease. By minimizing the physical trauma to the patient, peripheral interventions can reduce infection rates and recovery time as well as shorten hospital stays.
Alexander Margulis coined the term "interventional" for these new, minimally invasive techniques. He emphasized that to continue to be on the forefront of innovation, interventional radiologists must possess special training, technical skill, clinical knowledge, ability to care for patients, and closely collaborate with surgeons and internal medicine subspecialists.
Development of stents began slowly. In 1969, Dotter conceived the idea of expandable
stents with an intra-arterial coil spring. The first stents developed by Dotter and Andrew Craig were made of nitinol. Gianturco introduced his self-expandable Z stent. Hans Wallsten introduced a self-expandable mesh stent, Ernst Strecker a knitted tantalum stent and Julio Palmaz his balloon expandable stent, which was later perfected and introduced to clinical practice. Angioplasty and stenting revolutionized medicine and led the way for the more widely known applications of coronary artery angioplasty and stenting that revolutionized the practice of cardiology.
Treatment of GI bleeding has a storied tradition. After introduction of selective vasoconstrictive infusions by Baum, Josef Rösch introduced selective arterial embolization for treatment of uncontrollable bleeding in the early 70s. Anders Lundequist treated variceal bleeding with the technique of transhepatic variceal embolization in the mid 70s. Interventions in the biliary tract were developed by several pioneers. Interventional Radiologist Joachim Burrhenne invented and perfected the technique of percutaneous removal of retained biliary stones. Plinio Rossi and Hall Coons enriched biliary interventions with their work using biliary stents. The innovative interventionalists Kurt Amplatz, Willi Castaneda and Dave Hunter pioneered percutaneous uroradiologic interventions. They popularized nephrostomy drainage, percutaneous stone extraction, and urethral stenting.
The field of interventional oncology was pioneered by IR legends. Bob White pioneered embolization techniques for pulmonary AVMs. Sid Wallace was one of the first to treat bone and kidney tumors by embolization and treatment of disseminated liver metastases.
Today many conditions that once required surgery can be treated nonsurgically by interventional radiologists. Through a small knick in the skin, they use tiny catheters and miniature instruments so small they can be run through a person’s network of arteries to treat at the site of illness internally, saving the patient from open invasive surgery. While no treatment is risk free, the risks of interventional procedures are far lower than the risks of open surgery, and are a major advance in medicine for patients.
1966 Embolization therapy to treat tumors and spinal cord vascular malformations by blocking the blood flow
1967 The Judkins technique of coronary angiography, the technique still most widely used around the world today
1967 Closure of the patent ductus arteriosis, a heart defect in newborns of a vascular opening between the pulmonary artery and the aorta
1967 Selective vasoconstriction infusions for hemorrhage, now commonly used for bleeding ulcers, GI bleeding and arterial bleeding
1969 The catheter-delivered stenting technique and prototype stent
1960-74 Tools for interventions such as heparinized guidewires, contrast injector, disposable catheter needles and see-through film changer
1970’s Percutaneous removal of common bile duct stones
1970’s Occlusive coils
1972 Selective arterial embolization for GI bleeding, which was adapted to treat massive bleeding in other arteries in the body and to block blood supply to tumors
1973 Embolization for pelvic trauma
1974 Selective arterial thrombolysis for arterial occlusions, now used to treat blood clots, stroke, DVT, etc.
1974 Transhepatic embolization for variceal bleeding
1977-78 Embolization technique for pulmonary arteriovenous malformations and varicoceles
1977-83 Bland- and chemo-embolization for treatment of hepatocellular cancer and disseminated liver metastases
1980 Cryoablation to freeze liver tumors
1980 Development of special tools and devices for biliary manipulation
1980’s Biliary stents to allow bile to flow from the liver saving patients from biliary bypass surgery
1981 Embolization technique for spleen trauma
1982 TIPS (transjugular intrahepatic portosystemic shunt) to improve blood flow in damaged livers from conditions such as cirrhosis and hepatitis C
1982 Dilators for interventional urology, percutaneous removal of kidney stones
1983 The balloon-expandable stent (peripheral) used today
1985 Self-expanding stents
1990 Percutaneous extraction of gallbladder stones
1990 Radiofrequency ablation (RFA) technique for liver tumors
1990’s Treatment of bone and kidney tumors by embolization
1990’s RFA for soft tissue tumors, i.e., bone, breast, kidney, lung and liver cancer
1991 Abdominal aortic stent grafts
1994 The balloon-expandable coronary stent used today
1997 Intra-arterial delivery of tumor-killing viruses and gene therapy vectors to the liver
1999 Percutaneous delivery of pancreatic islet cells to the liver for transplantation to treat diabetes
1999 Developed the endovenous laser ablation procedure to treat varicose veins and venous disease
With the evolving need to train more clinically oriented interventionists, two alternative pathways to achieve certification in IR have been established through the leadership of the Society of Interventional Radiology
(SIR).
The DIRECT (Diagnostic and Interventional Radiology Enhanced Clinical Training) pathway allows for up to two years of clinical training prior entering the program. Therefore, residents may enter the new pathway from medical school or after two or more years of clinical training in other specialties such as internal medicine or vascular surgery. The core diagnostic training is 27 months in duration, with 21 total months of VIR training for a total of 48 months (four year) duration. The advantage of the DIRECT pathway is that upon successful completion of the program and 12 months of clinical practice, a clinician can achieve both a Diagnostic Radiology board certification and a subspecialty vascular IR certificate. The American Board of Radiology offers a complete list of programs that offer this pathway at: http://theabr.org/ic/ic_other/ic_direct.html.
An integrated Clinical Pathway has been created to provide breadth and depth of clinical experience for trainees who desire a primary career focusing on VIR rather than diagnostic radiology. The 6 year program allows for 29 months of Diagnostic Radiology training, 19 months of clinical training (including a medicine or surgery intern year) and research, and 21 months of VIR fellowship training. The Clinical Pathway is offered by institutions such as UVA, Northwestern and Brigham and Women's Hospital. The Clinical Pathway allows for certification in VIR and for board certification in diagnostic radiology.
For both the DIRECT and Clinical pathway
s, the SIR states that the trainee must become proficient to manage the inpatient and outpatient pre and post procedural clinical care and follow-up for all disease processes pertinent to the practice of VIR.
A newer Dual Certificate program has just been approved for implementation which is a six year curriculum, similar to the Clinical Pathway, that provides training for Board Certification in Diagnostic and Interventional Radiology.
, computed tomography (CT), ultrasound
(US), and magnetic resonance imaging
(MRI). Fluoroscopy and computed tomography use ionizing radiation
that may be potentially harmful to the patient and the interventional radiologist. However, both methods have the advantages of being fast and geometrically accurate. Ultrasound suffers from image quality and tissue contrast problems, but is also fast and inexpensive. Magnetic resonance imaging provides superior tissue contrast, at the cost of being expensive and requiring specialized instruments that will not interact with the magnetic fields present in the imaging volume.
Radiology
Radiology is a medical specialty that employs the use of imaging to both diagnose and treat disease visualized within the human body. Radiologists use an array of imaging technologies to diagnose or treat diseases...
, in which image-guided procedures are used to diagnose and treat a multitude of diseases across all body systems. Interventional radiologists are board-certified physicians who specialize in these minimally invasive, targeted treatments. They offer the most in-depth knowledge of the least invasive treatments available coupled with diagnostic and clinical experience across all specialties. They use X-rays, CT, ultrasound, MRI and other imaging modalities to advance a catheter or probe in the body to treat at the source of the disease non-surgically. As the inventors of angioplasty and the catheter-delivered stent, which were first used in the legs to treat peripheral arterial disease, interventional radiologists are the pioneers of minimally invasive modern medicine.
Today many conditions that once required surgery can be treated nonsurgically by interventional radiologists. Some of these procedures are done for purely diagnostic purposes (e.g., angiogram
Angiogram
Angiography or arteriography is a medical imaging technique used to visualize the inside, or lumen, of blood vessels and organs of the body, with particular interest in the arteries, veins and the heart chambers...
), while others are done for treatment purposes (e.g., angioplasty
Angioplasty
Angioplasty is the technique of mechanically widening a narrowed or obstructed blood vessel, the latter typically being a result of atherosclerosis. An empty and collapsed balloon on a guide wire, known as a balloon catheter, is passed into the narrowed locations and then inflated to a fixed size...
). Interventional radiology treatments offer less risk, pain, and recovery time compared to open surgery.
The basic concept behind interventional radiology is to diagnose or treat pathology using the least invasive technique possible. Images are used to direct interventional procedures, which are usually done with needles and narrow tubes called catheter
Catheter
In medicine, a catheter is a tube that can be inserted into a body cavity, duct, or vessel. Catheters thereby allow drainage, administration of fluids or gases, or access by surgical instruments. The process of inserting a catheter is catheterization...
s. The images provide road maps that allow the interventional radiologist to guide these instruments through the body to the areas containing disease. By minimizing the physical trauma to the patient, peripheral interventions can reduce infection rates and recovery time as well as shorten hospital stays.
History
Interventional radiologists are minimally invasive specialists. The landscape of medicine is constantly changing, and for the past 30 years, interventional radiologists have been responsible for much of the medical innovation and development of the minimally invasive procedures that are commonplace today. Interventional radiologists pioneered modern medicine with the invention of angioplasty and the catheter-delivered stent, which were first used to treat peripheral arterial disease. By using a catheter to open the blocked artery, the procedure allowed an 82-year-old woman, who refused amputation surgery, to keep her gangrene-ravaged left foot. To her surgeon’s disbelief, her pain ceased, she started walking, and three "irreversibly" gangrenous toes spontaneously sloughed. She left the hospital on her feet—both of them. The growth of interventional radiology was fueled by ties between interventionalists such as Charles Dotter and innovative device manufacturers like Bill Cook. Interventional radiologist Charles Dotter, MD, known as the "Father of Interventional Radiology" for pioneering this technique, was nominated for the Nobel Prize in Physiology or Medicine in 1978.Alexander Margulis coined the term "interventional" for these new, minimally invasive techniques. He emphasized that to continue to be on the forefront of innovation, interventional radiologists must possess special training, technical skill, clinical knowledge, ability to care for patients, and closely collaborate with surgeons and internal medicine subspecialists.
Development of stents began slowly. In 1969, Dotter conceived the idea of expandable
stents with an intra-arterial coil spring. The first stents developed by Dotter and Andrew Craig were made of nitinol. Gianturco introduced his self-expandable Z stent. Hans Wallsten introduced a self-expandable mesh stent, Ernst Strecker a knitted tantalum stent and Julio Palmaz his balloon expandable stent, which was later perfected and introduced to clinical practice. Angioplasty and stenting revolutionized medicine and led the way for the more widely known applications of coronary artery angioplasty and stenting that revolutionized the practice of cardiology.
Treatment of GI bleeding has a storied tradition. After introduction of selective vasoconstrictive infusions by Baum, Josef Rösch introduced selective arterial embolization for treatment of uncontrollable bleeding in the early 70s. Anders Lundequist treated variceal bleeding with the technique of transhepatic variceal embolization in the mid 70s. Interventions in the biliary tract were developed by several pioneers. Interventional Radiologist Joachim Burrhenne invented and perfected the technique of percutaneous removal of retained biliary stones. Plinio Rossi and Hall Coons enriched biliary interventions with their work using biliary stents. The innovative interventionalists Kurt Amplatz, Willi Castaneda and Dave Hunter pioneered percutaneous uroradiologic interventions. They popularized nephrostomy drainage, percutaneous stone extraction, and urethral stenting.
The field of interventional oncology was pioneered by IR legends. Bob White pioneered embolization techniques for pulmonary AVMs. Sid Wallace was one of the first to treat bone and kidney tumors by embolization and treatment of disseminated liver metastases.
Today many conditions that once required surgery can be treated nonsurgically by interventional radiologists. Through a small knick in the skin, they use tiny catheters and miniature instruments so small they can be run through a person’s network of arteries to treat at the site of illness internally, saving the patient from open invasive surgery. While no treatment is risk free, the risks of interventional procedures are far lower than the risks of open surgery, and are a major advance in medicine for patients.
Milestones Pioneered by Interventional Radiologists
1964 Angioplasty1966 Embolization therapy to treat tumors and spinal cord vascular malformations by blocking the blood flow
1967 The Judkins technique of coronary angiography, the technique still most widely used around the world today
1967 Closure of the patent ductus arteriosis, a heart defect in newborns of a vascular opening between the pulmonary artery and the aorta
1967 Selective vasoconstriction infusions for hemorrhage, now commonly used for bleeding ulcers, GI bleeding and arterial bleeding
1969 The catheter-delivered stenting technique and prototype stent
1960-74 Tools for interventions such as heparinized guidewires, contrast injector, disposable catheter needles and see-through film changer
1970’s Percutaneous removal of common bile duct stones
1970’s Occlusive coils
1972 Selective arterial embolization for GI bleeding, which was adapted to treat massive bleeding in other arteries in the body and to block blood supply to tumors
1973 Embolization for pelvic trauma
1974 Selective arterial thrombolysis for arterial occlusions, now used to treat blood clots, stroke, DVT, etc.
1974 Transhepatic embolization for variceal bleeding
1977-78 Embolization technique for pulmonary arteriovenous malformations and varicoceles
1977-83 Bland- and chemo-embolization for treatment of hepatocellular cancer and disseminated liver metastases
1980 Cryoablation to freeze liver tumors
1980 Development of special tools and devices for biliary manipulation
1980’s Biliary stents to allow bile to flow from the liver saving patients from biliary bypass surgery
1981 Embolization technique for spleen trauma
1982 TIPS (transjugular intrahepatic portosystemic shunt) to improve blood flow in damaged livers from conditions such as cirrhosis and hepatitis C
1982 Dilators for interventional urology, percutaneous removal of kidney stones
1983 The balloon-expandable stent (peripheral) used today
1985 Self-expanding stents
1990 Percutaneous extraction of gallbladder stones
1990 Radiofrequency ablation (RFA) technique for liver tumors
1990’s Treatment of bone and kidney tumors by embolization
1990’s RFA for soft tissue tumors, i.e., bone, breast, kidney, lung and liver cancer
1991 Abdominal aortic stent grafts
1994 The balloon-expandable coronary stent used today
1997 Intra-arterial delivery of tumor-killing viruses and gene therapy vectors to the liver
1999 Percutaneous delivery of pancreatic islet cells to the liver for transplantation to treat diabetes
1999 Developed the endovenous laser ablation procedure to treat varicose veins and venous disease
Training
As in most medical specialties, training varies depending on varying rules and regulations from country to country. In the United States, interventional radiologists are physicians whose education and training traditionally includes completing a college degree, four years of medical school, a year of training in general medicine and/or surgery (internship), a four year diagnostic radiology residency program, and then a one or two year fellowship in vascular & interventional radiology.With the evolving need to train more clinically oriented interventionists, two alternative pathways to achieve certification in IR have been established through the leadership of the Society of Interventional Radiology
Society of Interventional Radiology
The Society of Interventional Radiology is an American national organization of physicians, scientists and allied health professionals dedicated to improving public health through the use of minimally invasive, image-guided therapeutic interventions for disease management.It was founded in 1973 as...
(SIR).
The DIRECT (Diagnostic and Interventional Radiology Enhanced Clinical Training) pathway allows for up to two years of clinical training prior entering the program. Therefore, residents may enter the new pathway from medical school or after two or more years of clinical training in other specialties such as internal medicine or vascular surgery. The core diagnostic training is 27 months in duration, with 21 total months of VIR training for a total of 48 months (four year) duration. The advantage of the DIRECT pathway is that upon successful completion of the program and 12 months of clinical practice, a clinician can achieve both a Diagnostic Radiology board certification and a subspecialty vascular IR certificate. The American Board of Radiology offers a complete list of programs that offer this pathway at: http://theabr.org/ic/ic_other/ic_direct.html.
An integrated Clinical Pathway has been created to provide breadth and depth of clinical experience for trainees who desire a primary career focusing on VIR rather than diagnostic radiology. The 6 year program allows for 29 months of Diagnostic Radiology training, 19 months of clinical training (including a medicine or surgery intern year) and research, and 21 months of VIR fellowship training. The Clinical Pathway is offered by institutions such as UVA, Northwestern and Brigham and Women's Hospital. The Clinical Pathway allows for certification in VIR and for board certification in diagnostic radiology.
For both the DIRECT and Clinical pathway
Clinical Pathway
Clinical pathways, also known as care pathways, critical pathways, integrated care pathways, or care maps, are one of the main tools used to manage the quality in healthcare concerning the standardization of care processes. It has been proven that their implementation reduces the variability in...
s, the SIR states that the trainee must become proficient to manage the inpatient and outpatient pre and post procedural clinical care and follow-up for all disease processes pertinent to the practice of VIR.
A newer Dual Certificate program has just been approved for implementation which is a six year curriculum, similar to the Clinical Pathway, that provides training for Board Certification in Diagnostic and Interventional Radiology.
Imaging Modalities
Common interventional imaging modalities include fluoroscopyFluoroscopy
Fluoroscopy is an imaging technique commonly used by physicians to obtain real-time moving images of the internal structures of a patient through the use of a fluoroscope. In its simplest form, a fluoroscope consists of an X-ray source and fluorescent screen between which a patient is placed...
, computed tomography (CT), ultrasound
Medical ultrasonography
Diagnostic sonography is an ultrasound-based diagnostic imaging technique used for visualizing subcutaneous body structures including tendons, muscles, joints, vessels and internal organs for possible pathology or lesions...
(US), and magnetic resonance imaging
Magnetic resonance imaging
Magnetic resonance imaging , nuclear magnetic resonance imaging , or magnetic resonance tomography is a medical imaging technique used in radiology to visualize detailed internal structures...
(MRI). Fluoroscopy and computed tomography use ionizing radiation
Ionizing radiation
Ionizing radiation is radiation composed of particles that individually have sufficient energy to remove an electron from an atom or molecule. This ionization produces free radicals, which are atoms or molecules containing unpaired electrons...
that may be potentially harmful to the patient and the interventional radiologist. However, both methods have the advantages of being fast and geometrically accurate. Ultrasound suffers from image quality and tissue contrast problems, but is also fast and inexpensive. Magnetic resonance imaging provides superior tissue contrast, at the cost of being expensive and requiring specialized instruments that will not interact with the magnetic fields present in the imaging volume.
Procedures
Common IR procedures are:- Angiography: imaging the blood vessels to look for abnormalities with the use of various contrast media, including iodinated contrast, gadolinium based agents, and CO2 gas.
- Balloon angioplasty/stentAngioplastyAngioplasty is the technique of mechanically widening a narrowed or obstructed blood vessel, the latter typically being a result of atherosclerosis. An empty and collapsed balloon on a guide wire, known as a balloon catheter, is passed into the narrowed locations and then inflated to a fixed size...
: opening of narrow or blocked blood vessels using a balloon; may include placement of metallic stents as well (both self-expandingSelf-expandable metallic stentA self-expandable metallic stent is a metallic tube, or stent, used in order to hold open a structure in the gastrointestinal tract in order to allow the passage of food, chyme, stool, or other secretions required for digestion...
and balloon expandable).
- CholecystostomyCholecystostomyA cholecystostomy is a procedure where a stoma is created in the gallbladder, which can facilitate placement of a tube for drainage....
: placement of a tube into the gallbladder to remove infected bile in patients with cholecystitis, an inflammation of the gallbladder, who are too frail or too sick to undergo surgery
- Drain insertions: placement of tubes into different parts of the body to drain fluids (e.g., abscess drains to remove pus, pleural drains)
- Endovascular aneurysm repairEndovascular aneurysm repairEVAR which stands for Endovascular Aneurysm Repair , is a type of Endovascular surgery used to treat an abdominal aortic aneurysm or Thoracic Aortic Aneurysm, the procedure then specifically termed TEVAR...
- EmbolizationEmbolizationEmbolization is a non-surgical, minimally-invasive procedure performed by an interventional radiologist and interventional neuroradiologists. It involves the selective occlusion of blood vessels by purposely introducing emboli.-Therapeutic applications:...
: blocking abnormal blood (artery) vessels (e.g., for the purpose of stopping bleeding) or organs (to stop the extra function e.g. embolization of the spleen for hypersplenism) including uterine artery embolizationUterine artery embolizationUterine artery embolization is a procedure where an interventional radiologist uses a catheter to deliver small particles that block the blood supply to the uterine body...
for percutaneous treatment of uterine fibroids. Various embolic agents are used, including alcohol, glue, metallic coils, poly-viny alcohol particles, Embospheres, encapsulated chemo-microsphere, and gelfoam.- ChemoembolizationChemoembolizationChemoembolization is a procedure in which anticancer drugs are administered directly into a tumor through its feeding blood supply, with concurrent or subsequent blockage of the feeding vessel by occlusive agents that are injected through the delivery catheter...
: delivering cancer treatment directly to a tumour through its blood supply, then using clot-inducing substances to block the artery, ensuring that the delivered chemotherapy is not "washed out" by continued blood flow. - Radioembolization: Embolization of liver with radioactive microspheres of glass or plastic, to kill tumors while minimizing exposure to healthy cells.
- Chemoembolization
- ThrombolysisThrombolysisThrombolysis is the breakdown of blood clots by pharmacological means. It is colloquially referred to as clot busting for this reason...
: treatment aimed at dissolving blood clots (e.g., pulmonary emboli, leg vein thrombi, thrombosed hemodialysis accesses) with both pharmaceutical (TPA) and mechanical means
- BiopsyBiopsyA biopsy is a medical test involving sampling of cells or tissues for examination. It is the medical removal of tissue from a living subject to determine the presence or extent of a disease. The tissue is generally examined under a microscope by a pathologist, and can also be analyzed chemically...
: taking of a tissue sample from the area of interest for pathological examination from a percutaneous or transjugular approach
- Radiofrequency ablationRadiofrequency ablationRadio frequency ablation is a medical procedure where part of the electrical conduction system of the heart, tumor or other dysfunctional tissue is ablated using the heat generated from the high frequency alternating current to treat a medical disorder...
(RF/RFA): localized destruction of tissue (e.g., tumours) by heating
- CryoablationCryoablationCryoablation is a process that uses extreme cold to remove tissue .Cryoablation is used in a variety of clinical applications using hollow needles through which cooled, thermally conductive, fluids are circulated...
- localized destruction of tissue by freezing
- Line insertion: Vascular access and management of specialized kinds of intravenous devices (IVs) (e.g. PIC lines, Hickman lineHickman lineA Hickman line is an intravenous catheter most often used for the administration of chemotherapy or other medications, as well as for the withdrawal of blood for analysis. Some types of Hickman lines are used mainly for the purpose of apheresis or dialysis...
s, subcutaneous ports including translumbar and transhepatic venous lines)
- IVC filters: - metallic filters placed in the inferior vena cavae to prevent propagation of deep venous thrombus, both temporary and permanent.
- VertebroplastyVertebroplastyVertebroplasty and kyphoplasty are similar medical spinal procedure where bone cement is injected through a small hole in the skin into a fractured vertebra with the goal of relieving the pain of vertebral compression fractures...
: percutaneousPercutaneousIn surgery, percutaneous pertains to any medical procedure where access to inner organs or other tissue is done via needle-puncture of the skin, rather than by using an "open" approach where inner organs or tissue are exposed .The percutaneous approach is commonly used in vascular procedures...
injection of biocompatible bone cement inside fractured vertebrae
- NephrostomyNephrostomyA nephrostomy is an artificial opening created between the kidney and the skin which allows for the urinary diversion directly from the upper part of the urinary system ....
placement: Placing a catheter directly into the kidney to drain urine in situations where normal flow of urine is obstructed. NUS catheters are nephroureteral stents which are placed through the ureter and into the bladder.
- Radiologically inserted gastrostomy or RIG: Placement of a feeding tube percutaneously into the stomach and/or jejunum.
- DialysisDialysisIn medicine, dialysis is a process for removing waste and excess water from the blood, and is primarily used to provide an artificial replacement for lost kidney function in people with renal failure...
access and related intervention: Placement of tunneled hemodialysis catheters, peritoneal dialysis catheters, and revision/thrombolysis of poorly functioning surgically placed AV fistulas and grafts.
- TIPSTransjugular intrahepatic portosystemic shuntA Transjugular Intrahepatic Portosystemic Shunt is an artificial channel within the liver that establishes communication between the inflow portal vein and the outflow hepatic vein...
: Placement of a Transjugular Intrahepatic Porto-systemic Shunt (TIPS) for management of select patients with critical end-stage liver disease and portal hypertension
- Biliary intervention - Placement of catheters in the biliary system to bypass biliary obstructions and decompress the biliary system. Also placement of permanent indwelling biliary stents.
- Endovenous laser treatmentEndovenous laser treatmentEndovenous laser treatment is a minimally invasive ultrasound-guided technique used for treating varicose veins using laser energy.-Methods:...
of varicose veins - Placement of thin laser fiber in varicose veins for non-surgical treatment of venous insufficiency
Tools
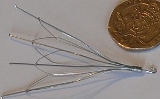
There are a number of catheters used in interventional radiology that can be loosely divided into five types:- Diagnostic angiographic catheters
- Micro catheters
- Drainage catheters
- Balloon catheterBalloon catheterA balloon catheter is a type of "soft" catheter with an inflatable "balloon" at its tip which is used during a catheterization procedure to enlarge a narrow opening or passage within the body...
s
- Central venous catheterCentral venous catheterIn medicine, a central venous catheter is a catheter placed into a large vein in the neck , chest or groin...
s
See also
- Interventional neuroradiologyInterventional neuroradiologyInterventional Neuroradiology /Neurointerventional Surgery is an Accreditation Council for Graduate Medical Education accredited medical subspecialty specializing in minimally invasive image-based technologies and procedures used in diagnosis and treatment of diseases of the head, neck, and...
- MRI RobotMRI RobotAn MRI robot is a medical robot capable of operating within a magnetic resonance imaging scanner for the purpose of performing or assisting in image-guided interventions ....
: MRI Stealth Robot Technology - URobotics: New technologies for image-guided intervention
- Radiation protection

