
Electronic Health Record
Encyclopedia
An electronic health record (EHR) (also electronic patient record (EPR) or computerised patient record) is an evolving concept defined as a systematic collection of electronic health information about individual patients or populations. It is a record in digital format that is capable of being shared across different health care settings, by being embedded in network-connected enterprise-wide information systems. Such records may include a whole range of data in comprehensive or summary form, including demographics
Demographics
Demographics are the most recent statistical characteristics of a population. These types of data are used widely in sociology , public policy, and marketing. Commonly examined demographics include gender, race, age, disabilities, mobility, home ownership, employment status, and even location...
, medical history, medication and allergies, immunization
Immunization
Immunization, or immunisation, is the process by which an individual's immune system becomes fortified against an agent ....
status, laboratory test results, radiology images, vital signs, personal stats like age and weight, and billing information.
Its purpose can be understood as a complete record of patient encounters that allows the automation and streamlining of the workflow in health care settings and increases safety through evidence-based decision support, quality management, and outcomes reporting.
Terminology
The terms EHR, EPR and EMR (electronic medical record)Electronic medical record
An electronic medical record is a computerized medical record created in an organization that delivers care, such as a hospital or physician's office...
are often used interchangeably, although a difference between them can be defined. The EMR can be defined as the legal patient record created in hospitals and ambulatory environments that is the data source for the EHR. It is important to note that an EHR is generated and maintained within an institution, such as a hospital, integrated delivery network, clinic, or physician office, to give patients, physicians and other health care providers, employers, and payers or insurers access to a patient's medical records across facilities.
A personal health record
Personal health record
A personal health record or PHR is a health record where health data is curated by an individual user themselves. This stands in contrast with the more widely used electronic medical record which is held by institutions such as a hospital and contains data entered by clinicians or billing data in...
is, in modern parlance, generally defined as an EHR that the individual patient controls.
Philosophical views of the EHR
Within a meta-narrative systematic reviewSystematic review
A systematic review is a literature review focused on a research question that tries to identify, appraise, select and synthesize all high quality research evidence relevant to that question. Systematic reviews of high-quality randomized controlled trials are crucial to evidence-based medicine...
of research in the field, Prof. Trish Greenhalgh and colleagues defined a number of different philosophical approaches to the EHR. The health information systems literature has seen the EHR as a container holding information about the patient, and a tool for aggregating clinical data for secondary uses (billing, audit etc.). However, other research traditions see the EHR as a contextualised artifact within a socio-technical system. For example, actor-network theory
Actor-network theory
Actor–network theory, often abbreviated as ANT, is a distinctive approach to social theory and research which originated in the field of science studies...
would see the EHR as an actant in a network (e.g. ), while research in computer supported cooperative work
Computer supported cooperative work
The term computer-supported cooperative work was first coined by Irene Greif and Paul M. Cashman in 1984, at a workshop attended by individuals interested in using technology to support people in their work. At about this same time, in 1987 Dr...
(CSCW) sees the EHR as a tool supporting particular work. Prof. Barry Robson and OK Baek also reviewed these aspects and see the EHR as pivotal in human history.
Advantages
Several possible advantages to EHRs over paper records have been proposed, but there is debate about the degree to which these are achieved in practice (e.g. ).Reduction of cost
In the U.S. a vast amount of funds are allocated towards the health care industry—more than $1.7 trillion per year. If savings are allocated using the current level of spending from the National Health Accounts, Medicare would receive about $23 billion of the potential savings per year, and private payers would receive $31 billion per year.Improve quality of care
The implementation of electronic health records (EHR) can help lessen patient sufferance due to medical errors and the inability of analysts to assess quality. Information Technology is being used today to automate day-to-day processes, thus helping to reduce administration costs which then in turn can free up time and money for patient care.EHR systems can help reduce medical errors by providing healthcare workers with decision support. Fast access to medical literature and current best practices in medicine are hypothesised to enable proliferation of ongoing improvements in healthcare efficacy. Improved usage of EHR is achieved if the presentation on screen or on paper is not just longitudinal, but hierarchically ordered and layered.
During compilation while hospitalisation or ambulant serving of the patient, easing to get access on details is improved with browser capabilities applied to screen presentations also cross referring to the respective coding concepts ICD
ICD
The International Statistical Classification of Diseases and Related Health Problems is a medical classification that provides codes to classify diseases and a wide variety of signs, symptoms, abnormal findings, complaints, social circumstances, and external causes of injury or disease...
, DRG
DRG
DRG, a three-letter acronym, may refer to:* DRG London, a Digital Audio Broadcasting multiplex available in the London area* DRG Technologies, a company based in Safford, Arizona...
and medical procedures information.
Computerized Physician Order Entry (CPOE)—one component of EHR—increases patient safety by listing instructions for physicians to follow when they prescribe drugs to patients. Naturally, CPOE can tremendously decrease medical errors: CPOE could eliminate 200,000 adverse drug events and save about $1 billion per year if installed in all hospitals.
Promote evidence-based medicine
EHRs provide access to unprecedented amounts of clinical data for research that can accelerate the level of knowledge of effective medical practices.Realistically, these benefits may only be realized if the EHR systems are interoperable and wide spread (for example, national or regional level) so that various systems can easily share information. Also, to avoid failures that can cause injury to the patient and violations to privacy, the best practices in software engineering and medical informatics must be deployed.
Record keeping and mobility
EHR systems have the advantages of being able to connect to many electronic medical record systems. In the current global medical environment, patients are shopping for their procedures. Many international patients travel to US cities with academic research centers for specialty treatment or to participate in Clinical Trials. Coordinating these appointments via paper records is a time-consuming procedure.Disadvantages
Critics point out that while EHRs may save the "health system" money, physicians, those who buy the systems, may not benefit financially. EHR price tags range widely, depending on what's included, how robust the system is, and how many providers use it. Asked what they paid in an online survey, about a third of respondents paid between $500 and $3,000 per physician. A third paid between $3,001 and $6,000, and 33 percent paid more than $6,000 per physician for their EHR. Physicians do tend to see at least short-term decreases in productivity as they implement an EHR. They spend more time entering data into an empty EHR than they used to spend updating a paper chart with a simple dictation. Such hurdles can be overcome once the software has some data, as physicians learn to use templates for data entry, and as workflow in the practice changes, but not every practice gets that far.Studies also call into question whether, in real life, EHRs improve quality. 2009 produced several articles raising doubts about EHR benefits.
Costs
The steep price of EHR and provider uncertainty regarding the value they will derive from adoption in the form of return on investment has a significant influence on EHR adoption. In a project initiated by the Office of the National Coordinator for Health Information (ONC), surveyors found that hospital administrators and physicians who had adopted EHR noted that any gains in efficiency were offset by reduced productivity as the technology was implemented, as well as the need to increase information technology staff to maintain the system.The U.S. Congressional Budget Office concluded that the cost savings may occur only in large integrated institutions like Kaiser Permanente, and not in small physician offices. They challenged the Rand Corp. estimates of savings. "Office-based physicians in particular may see no benefit if they purchase such a product—and may even suffer financial harm. Even though the use of health IT could generate cost savings for the health system at large that might offset the EHR's cost, many physicians might not be able to reduce their office expenses or increase their revenue sufficiently to pay for it. For example. the use of health IT could reduce the number of duplicated diagnostic tests. However, that improvement in efficiency would be unlikely to increase the income of many physicians." One CEO of a EHR company has argued if a physician performs tests in the office, it might reduce his or her income. "Given the ease at which information can be exchanged between health IT systems, patients whose physicians use them may feel that their privacy is more at risk than if paper records were used."
Time
Often, doctors do not want to spend the time to learn a new system. Some doctors believe that adopting a system with EHRs could reduce clinical productivity.Privacy concerns
In the United States, Great Britain, and Germany, the concept of a national centralized server model of healthcare data has been poorly received. Issues of privacy and security in such a model have been of concern.Privacy concerns in healthcare apply to both paper and electronic records. According to the Los Angeles Times, roughly 150 people (from doctors and nurses to technicians and billing clerks) have access to at least part of a patient's records during a hospitalization, and 600,000 payers, providers and other entities that handle providers' billing data have some access also. Recent revelations of "secure" data breaches at centralized data repositories, in banking and other financial institutions, in the retail industry, and from government database
Government database
Government databases collect personal information for various reasons .-Canada:...
s, have caused concern about storing electronic medical records in a central location. Records that are exchanged over the Internet are subject to the same security concerns as any other type of data transaction over the Internet.
The Health Insurance Portability and Accountability Act (HIPAA)
Health Insurance Portability and Accountability Act
The Health Insurance Portability and Accountability Act of 1996 was enacted by the U.S. Congress and signed by President Bill Clinton in 1996. It was originally sponsored by Sen. Edward Kennedy and Sen. Nancy Kassebaum . Title I of HIPAA protects health insurance coverage for workers and their...
was passed in the US in 1996 to establish rules for access, authentications, storage and auditing, and transmittal of electronic medical records. This standard made restrictions for electronic records more stringent than those for paper records. However, there are concerns as to the adequacy of these standards.
In the European Union
European Union
The European Union is an economic and political union of 27 independent member states which are located primarily in Europe. The EU traces its origins from the European Coal and Steel Community and the European Economic Community , formed by six countries in 1958...
(EU), several Directives of the European Parliament and of the Council protect the processing and free movement of personal data, including for purposes of health care.
Personal Information Protection and Electronic Documents Act
Personal Information Protection and Electronic Documents Act
The Personal Information Protection and Electronic Documents Act is a Canadian law relating to data privacy. It governs how private sector organizations collect, use and disclose personal information in the course of commercial business. In addition, the Act contains various provisions to...
(PIPEDA) was given Royal Assent in Canada on April 13, 2000 to establish rules on the use, disclosure and collection of personal information. The personal information includes both non-digital and electronic form. In 2002, PIPEDA extended to the health sector in Stage 2 of the law's implementation. There are four provinces where this law does not apply because its privacy law was considered similar to PIPEDA: Alberta, British Columbia, Ontario and Quebec.
One major issue that has risen on the privacy of the US network for electronic health records is the strategy to secure the privacy of patients. Former US president Bush called for the creation of networks, but federal investigators report that there is no clear strategy to protect the privacy of patients as the promotions of the electronic medical records expands throughout the United States. In 2007, the Government Accountability Office reports that there is a “jumble of studies and vague policy statements but no overall strategy to ensure that privacy protections would be built into computer networks linking insurers, doctors, hospitals and other health care providers.”
The privacy threat posed by the interoperability of a national network is a key concern. One of the most vocal critics of EMRs, New York University Professor Jacob M. Appel, has claimed that the number of people who will need to have access to such a truly interoperable national system, which he estimates to be 12 million, will inevitable lead to breaches of privacy on a massive scale. Appel has written that while "hospitals keep careful tabs on who accesses the charts of VIP patients," they are powerless to act against "a meddlesome pharmacist in Alaska" who "looks up the urine toxicology on his daughter's fiance in Florida, to check if the fellow has a cocaine habit." This is a significant barrier for the adoption of an EHR. Accountability among all the parties that are involved in the processing of electronic transactions including the patient, physician office staff, and insurance companies, is the key to successful advancement of the EHR in the US Supporters of EHRs have argued that there needs to be a fundamental shift in “attitudes, awareness, habits, and capabilities in the areas of privacy and security” of individual’s health records if adoption of an EHR is to occur.
According to the Wall Street Journal, the DHHS takes no action on complaints under HIPAA, and medical records are disclosed under court orders in legal actions such as claims arising from automobile accidents. HIPAA has special restrictions on psychotherapy records, but psychotherapy records can also be disclosed without the client's knowledge or permission, according to the Journal. For example, Patricia Galvin, a lawyer in San Francisco, saw a psychologist at Stanford Hospital & Clinics after her fiance committed suicide. Her therapist had assured her that her records would be confidential. But after she applied for disability benefits, Stanford gave the insurer her therapy notes, and the insurer denied her benefits based on what Galvin claims was a misinterpretation of the notes. Stanford had merged her notes with her general medical record, and the general medical record wasn't covered by HIPAA restrictions.
Within the private sector, many companies are moving forward in the development, establishment and implementation of medical record banks and health information exchange.
By law, companies are required to follow all HIPAA standards and adopt the same information-handling practices that have been in effect for the federal government for years. This includes two ideas, standardized formatting of data electronically exchanged and federalization of security and privacy practices among the private sector.
Private companies have promised to have “stringent privacy policies and procedures.” If protection and security are not part of the systems developed, people will not trust the technology nor will they participate in it. So, the private sector know the importance of privacy and the security of the systems and continue to advance well ahead of the federal government with electronic health records.
Liability
Legal liability in all aspects of healthcare was an increasing problem in the 1990s and 2000s. The surge in the per capita number of attorneys and changes in the tortTort
A tort, in common law jurisdictions, is a wrong that involves a breach of a civil duty owed to someone else. It is differentiated from a crime, which involves a breach of a duty owed to society in general...
system caused an increase in the cost of every aspect of healthcare, and healthcare technology was no exception.
Failure or damages caused during installation or utilization of an EHR system has been feared as a threat in lawsuits. Similarly, it's important to recognize that the implementation of electronic health records carries with it significant legal risks.
This liability concern was of special concern for small EHR system makers. Some smaller companies may be forced to abandon markets based on the regional liability climate. Larger EHR providers (or government-sponsored providers of EHRs) are better able to withstand legal assaults.
In some communities, hospitals attempt to standardize EHR systems by providing discounted versions of the hospital's software to local healthcare providers. A challenge to this practice has been raised as being a violation of Stark rules that prohibit hospitals from preferentially assisting community healthcare providers. In 2006, however, exceptions to the Stark rule were enacted to allow hospitals to furnish software and training to community providers, mostly removing this legal obstacle.
Legal interoperability
In cross-border use cases of EHR implementations, the additional issue of legal interoperability arises. Different countries may have diverging legal requirements for the content or usage of electronic health records, which can require radical changes of the technical makeup of the EHR implementation in question. (especially when fundamental legal incompatibilities are involved) Exploring these issues is therefore often necessary when implementing cross-border EHR solutions.Regulatory compliance
- Consumer Credit Act 2006Consumer Credit Act 2006The Consumer Credit Act 2006 is an Act of the Parliament of the United Kingdom intended to increase consumer protection when borrowing money.-Provisions:...
- HIPAA
- Health Level 7Health Level 7Health Level Seven , is an all-volunteer, non-profit organization involved in development of international healthcare informatics interoperability standards...
Standards
- ANSI X12 (EDIElectronic Data InterchangeElectronic data interchange is the structured transmission of data between organizations by electronic means. It is used to transfer electronic documents or business data from one computer system to another computer system, i.e...
) - transaction protocols used for transmitting patient data. Popular in the United States for transmission of billingInvoiceAn invoice or bill is a commercial document issued by a seller to the buyer, indicating the products, quantities, and agreed prices for products or services the seller has provided the buyer. An invoice indicates the buyer must pay the seller, according to the payment terms...
data. - CENEuropean Committee for StandardizationThe European Committee for Standardization or Comité Européen de Normalisation , is a non-profit organisation whose mission is to foster the European economy in global trading, the welfare of European citizens and the environment by providing an efficient infrastructure to interested parties for...
's TC/251 provides EHR standards in Europe including:- EN 13606EN 13606The overall goal of this Health informatics - Electronic Health Record Communication European Standard is to define a rigorous and stable information architecture for communicating part or all of the Electronic Health Record of a single subject of care...
, communication standards for EHR information - CONTSYS (EN 13940), supports continuity of care record standardization.
- HISAHISAThe CEN Standard Architecture for Healthcare Information Systems , Health Informatics Service Architecture or HISA is a standard aimed at enabling the development modular open systems to support healthcare...
(EN 12967), a services standard for inter-system communication in a clinical information environment.
- EN 13606
- Continuity of Care RecordContinuity of Care RecordContinuity of Care Record is a health record standard specification developed jointly by ASTM International, the Massachusetts Medical Society , the Healthcare Information and Management Systems Society , the American Academy of Family Physicians , the American Academy of Pediatrics , and other...
- ASTM International Continuity of Care Record standard - DICOM - an international communications protocol standard for representing and transmitting radiology (and other) image-based data, sponsored by NEMANational Electrical Manufacturers Associationis the association of electrical and medical imaging equipment manufacturers. Founded in 1926 and headquartered near Washington, D.C., its approximately manufacture products used in the generation, transmission, distribution, control, and end use of electricity. These products are used in utility,...
(National Electrical Manufacturers Association) - HL7 - a standardized messaging and text communications protocol between hospital and physicianPhysicianA physician is a health care provider who practices the profession of medicine, which is concerned with promoting, maintaining or restoring human health through the study, diagnosis, and treatment of disease, injury and other physical and mental impairments...
record systems, and between practice management systems - ISO - ISO TC 215 provides international technical specifications for EHRs. ISO 18308 describes EHR architectures
The U.S. federal government has issued new rules of electronic health records.
Open Specifications
- openEHROpenehropenEHR is an open standard specification in health informatics that describes the management and storage, retrieval and exchange of health data in electronic health records . In openEHR, all health data for a person is stored in a "one lifetime", vendor-independent, person-centred EHR...
: an open community developed specification for a shared health record with web-based content developed online by experts. Strong multilingual capability. - Virtual Medical RecordVirtual Medical RecordThe Virtual Medical Record is a simplified, standardised electronic health record data model designed to support interfacing to clinical decision support systems.The project is sponsored by HL7....
: HL7's proposed model for interfacing with clinical decision support systems. - SMArt Platforms: an open platform specification to provide a standard base for healthcare applications.
Customization
Each healthcare environment functions differently, often in significant ways. It is difficult to create a "one-size-fits-all" EHR system.An ideal EHR system will have record standardization but interfaces that can be customized to each provider environment. Modularity in an EHR system facilitates this. Many EHR companies employ vendors to provide customization.
This customization can often be done so that a physician's input interface closely mimics previously utilized paper forms.
At the same time they reported negative effects in communication, increased overtime, and missing records when a non-customized EMR system was utilized. Customizing the software when it is released yields the highest benefits because it is adapted for the users and tailored to workflows specific to the institution.
Customization can have its disadvantages. There is, of course, higher costs involved to implementation of a customized system initially. More time must be spent by both the implementation team and the healthcare provider to understand the workflow needs.
Development and maintenance of these interfaces and customizations can also lead to higher software implementation and maintenance costs.
Long-term preservation and storage of records
An important consideration in the process of developing electronic health records is to plan for the long-term preservation and storage of these records. The field will need to come to consensus on the length of time to store EHRs, methods to ensure the future accessibility and compatibility of archived data with yet-to-be developed retrieval systems, and how to ensure the physical and virtual security of the archives.Additionally, considerations about long-term storage of electronic health records are complicated by the possibility that the records might one day be used longitudinally and integrated across sites of care. Records have the potential to be created, used, edited, and viewed by multiple independent entities. These entities include, but are not limited to, primary care physicians, hospitals, insurance companies, and patients. Mandl et al. have noted that “choices about the structure and ownership of these records will have profound impact on the accessibility and privacy of patient information.”
The required length of storage of an individual electronic health record will depend on national and state regulations, which are subject to change over time. Ruotsalainen and Manning have found that the typical preservation time of patient data varies between 20 and 100 years. In one example of how an EHR archive might function, their research "describes a co-operative trusted notary archive (TNA) which receives health data from different EHR-systems, stores data together with associated meta-information for long periods and distributes EHR-data objects. TNA can store objects in XML-format and prove the integrity of stored data with the help of event records, timestamps and archive e-signatures."
In addition to the TNA archive described by Ruotsalainen and Manning, other combinations of EHR systems and archive systems are possible. Again, overall requirements for the design and security of the system and its archive will vary and must function under ethical and legal principles specific to the time and place.
While it is currently unknown precisely how long EHRs will be preserved, it is certain that length of time will exceed the average shelf-life of paper records. The evolution of technology is such that the programs and systems used to input information will likely not be available to a user who desires to examine archived data. One proposed solution to the challenge of long-term accessibility and usability of data by future systems is to standardize information fields in a time-invariant way, such as with XML language. Olhede and Peterson report that “the basic XML-format has undergone preliminary testing in Europe by a Spri project and been found suitable for EU purposes. Spri has advised the Swedish National Board of Health and Welfare and the Swedish National Archive to issue directives concerning the use of XML as the archive-format for EHCR (Electronic Health Care Record) information."
Synchronization of records
When care is provided at two different facilities, it may be difficult to update records at both locations in a co-ordinated fashion.Two models have been used to satisfy this problem: a centralized data server solution, and a peer-to-peer file synchronization
File synchronization
File synchronization in computing is the process of ensuring that computer files in two or more locations are updated via certain rules....
program (as has been developed for other peer-to-peer networks
Peer-to-peer
Peer-to-peer computing or networking is a distributed application architecture that partitions tasks or workloads among peers. Peers are equally privileged, equipotent participants in the application...
).
Synchronization programs for distributed storage models, however, are only useful once record standardization has occurred.
Merging of already existing public healthcare databases is a common software challenge. The ability of electronic health record systems to provide this function is a key benefit and can improve healthcare delivery.
eHealth and teleradiology
The sharing of patient information between health care organizations and IT systems is changing from a "point to point" model to a "many to many" one. The European Commission is supporting moves to facilitate cross-border interoperability of e-health systems and to remove potential legal hurdles, as in the project www.epsos.eu/. To allow for global shared workflow, studies will be locked when they are being read and then unlocked and updated once reading is complete. Radiologists will be able to serve multiple health care facilities and read and report across large geographical areas, thus balancing workloads. The biggest challenges will relate to interoperability and legal clarity. In some countries it is almost forbidden to practice teleradiology. The variety of languages spoken is a problem and multilingual reporting templates for all anatomical regions are not yet available. However, the market for e-health and teleradiology is evolving more rapidly than any laws or regulations.United States
In a 2008 survey by DesRoches et al. of 4484 physicians (62% response rate), 83% of all physicians, 80% of primary care physicians, and 86% of non-primary care physicians had no EHRs. "Among the 83% of respondents who did not have electronic health records, 16%" had bought, but not implemented an EHR system yet.The 2009 National Ambulatory Medical Care Survey of 5200 physicians (70% response rate) by the National Center for Health Statistics
National Center for Health Statistics
National Center for Health Statistics is a division of the United States federal agency the Centers for Disease Control and Prevention . As such, NCHS is under the United States Department of Health and Human Services...
showed that 51.7% of office-based physicians did not use any EMR/EHR system.
The healthcare industry spends only 2% of gross revenues on HIT, which is low compared to other information intensive industries such as finance, which spend upwards of 10%.
2009 HITECH Act
The Health Information Technologyfor Economic and Clinical Health Act (a part of the 2009 stimulus package
American Recovery and Reinvestment Act of 2009
The American Recovery and Reinvestment Act of 2009, abbreviated ARRA and commonly referred to as the Stimulus or The Recovery Act, is an economic stimulus package enacted by the 111th United States Congress in February 2009 and signed into law on February 17, 2009, by President Barack Obama.To...
) set meaningful use of interoperable EHR adoption in the health care system as a critical national goal and incentivized EHR adoption. The "goal is not adoption alone but 'meaningful use' of EHRs — that is, their use by providers to achieve significant improvements in care."
Title IV of the act promises maximum incentive payments for Medicaid
Medicaid
Medicaid is the United States health program for certain people and families with low incomes and resources. It is a means-tested program that is jointly funded by the state and federal governments, and is managed by the states. People served by Medicaid are U.S. citizens or legal permanent...
to those who adopt and use "certified EHRs" of $63,750 over 6 years beginning in 2011. Eligible professionals must begin receiving payments by 2016 to qualify for the program. For Medicare the maximum payments are $44,000 over 5 years. Doctors who do not adopt an EHR by 2015 will be penalized 1% of Medicare payments, increasing to 3% over 3 years. In order to receive the EHR stimulus money, the HITECH act (ARRA) requires doctors to show "meaningful use" of an EHR system. As of June 2010, there are no penalty provisions for Medicaid.
Health information exchange (HIE) has emerged as a core capability for hospitals and physicians to achieve "meaningful use" and receive stimulus funding. Healthcare vendors are pushing HIE as a way to allow EHR systems to pull disparate data and function on a more interoperable level.
Starting in 2015, hospitals and doctors will be subject to financial penalties under Medicare if they are not using electronic health records.
Meaningful use
The main components of Meaningful Use are:- The use of a certified EHR in a meaningful manner, such as e-prescribing.
- The use of certified EHR technology for electronic exchange of health information to improve quality of health care.
- The use of certified EHR technology to submit clinical quality and other measures.
In other words, providers need to show they're using certified EHR technology in ways that can be measured significantly in quality and in quantity.
The meaningful use of EHRs intended by the US government incentives is categorized as follows:
- Improve care coordination
- Reduce healthcare disparities
- Engage patients and their families
- Improve population and public health
- Ensure adequate privacy and security
The Obama Administration’s Health IT program intends to use federal investments to stimulate the market of electronic health records:
- Incentives: to providers who use IT
- Strict and open standards: To ensure users and sellers of EHRs work towards the same goal
- Certification of software: To provide assurance that the EHRs meet basic quality, safety, and efficiency standards
The detailed definition of “meaningful use” is to be rolled out in 3 stages over a period of time until 2015. Details of each stage are hotly debated by various groups. Only stage 1 has been defined while the remaining stages will evolve over time.
Meaningful use Stage 1
The first steps in achieving meaningful use are to have a certified electronic health record (EHR) and to be able to demonstrate that it is being used to meet the requirements. Stage 1 contains 25 objectives/measures for Eligible Providers (EPs) and 24 objectives/measures for eligible hospitals. The objectives/measures have been divided into a core set and menu set. EPs and eligible hospitals must meet all objectives/measures in the core set (15 for EPs and 14 for eligible hospitals). EPs must meet 5 of the 10 menu-set items during Stage 1.
Full list of the Core Requirements and a full list of the Menu Requirements.
Core Requirements:
- Use computerized order entry for medication orders.
- Implement drug-drug, drug-allergy checks.
- Generate and transmit permissible prescriptions electronically.
- Record demographics.
- Maintain an up-to-date problem list of current and active diagnoses.
- Maintain active medication list.
- Maintain active medication allergy list.
- Record and chart changes in vital signs.
- Record smoking status for patients 13 years old or older.
- Implement one clinical decision support rule.
- Report ambulatory quality measures to CMS or the States.
- Provide patients with an electronic copy of their health information upon request.
- Provide clinical summaries to patients for each office visit.
- Capability to exchange key clinical information electronically among providers and patient authorized entities.
- Protect electronic health information (privacy & security)
Menu Requirements:
- Implement drug-formulary checks.
- Incorporate clinical lab-test results into certified EHR as structured data.
- Generate lists of patients by specific conditions to use for quality improvement, reduction of disparities, research, and outreach.
- Send reminders to patients per patient preference for preventive/ follow-up care
- Provide patients with timely electronic access to their health information (including lab results, problem list, medication lists, allergies)
- Use certified EHR to identify patient-specific education resources and provide to patient if appropriate.
- Perform medication reconciliation as relevant
- Provide summary care record for transitions in care or referrals.
- Capability to submit electronic data to immunization registries and actual submission.
- Capability to provide electronic syndromic surveillance data to public health agencies and actual transmission.
Start-up costs
In a survey by DesRoches et al. (2008), 66% of physicians without EHRs cited capital costs as a barrier to adoption, while 50% were uncertain about the investment. Around 56% of physicians without EHRs stated that financial incentives to purchase and/or use EHRs would facilitate adoption. In 2002, initial costs were estimated to be $50,000–70,000 per physician in a 3-physician practice. Since then, costs have decreased with increasing adoption. A 2011 survey estimated a cost of $32,000 per physician in a 5-physician practice during the first 60 days of implementation.
One case study by Miller et al. (2005) of 14 small primary-care practices found that the average practice paid for the initial and ongoing costs within 2.5 years. A 2003 cost-benefit analysis found that using EMRs for 5 years created a net benefit of $86,000 per provider.
Some physicians are skeptical of the positive claims and believe the data is skewed by vendors and others with a interest in EHR implementation.
Brigham and Women’s Hospital in Boston, Massachusetts, estimated it achieved net savings of $5 million to $10 million per year following installation of a computerized physician order entry system that reduced serious medication errors by 55 percent. Another large hospital generated about $8.6 million in annual savings by replacing paper medical charts with EHRs for outpatients and about $2.8 million annually by establishing electronic access to laboratory results and reports.
Maintenance costs
Maintenance costs can be high. Miller et al. found the average estimated maintenance cost was $8500 per FTE
Full-time equivalent
Full-time equivalent , is a unit to measure employed persons or students in a way that makes them comparable although they may work or study a different number of hours per week. FTE is often used to measure a worker's involvement in a project, or to track cost reductions in an organization...
health-care provider per year.
Furthermore, software technology advances at a rapid pace. Most software systems require frequent updates, often at a significant ongoing cost. Some types of software and operating systems require full-scale re-implementation periodically, which disrupts not only the budget but also workflow. Costs for upgrades and associated regression testing can be particularly high where the applications are governed by FDA regulations (e.g. Clinical Laboratory systems). Physicians desire modular upgrades and ability to continually customize, without large-scale reimplementation.
Training costs
Training of employees to use an EHR system is costly, just as for training in the use of any other hospital system. New employees, permanent or temporary, will also require training as they are hired.
In the United States, a substantial majority of healthcare providers train at a VA facility sometime during their career. With the widespread adoption of the Veterans Health Information Systems and Technology Architecture (VistA
VistA
The Veterans Health Information Systems and Technology Architecture is an enterprise-wide information system built around an Electronic Health Record , used throughout the United States Department of Veterans Affairs medical system, known as the Veterans Health Administration .It's a collection...
) electronic health record system at all VA facilities, few recently-trained medical professionals will be inexperienced in electronic health record systems. Older practitioners who are less experienced in the use of electronic health record systems will retire over time.
Implementations
In the United States, the Department of Veterans AffairsUnited States Department of Veterans Affairs
The United States Department of Veterans Affairs is a government-run military veteran benefit system with Cabinet-level status. It is the United States government’s second largest department, after the United States Department of Defense...
(VA) has the largest enterprise-wide health information system that includes an electronic medical record, known as the Veterans Health Information Systems and Technology Architecture (VistA
VistA
The Veterans Health Information Systems and Technology Architecture is an enterprise-wide information system built around an Electronic Health Record , used throughout the United States Department of Veterans Affairs medical system, known as the Veterans Health Administration .It's a collection...
). A key component in VistA is their VistA imaging
Vista imaging
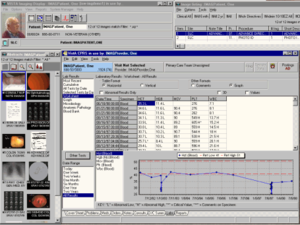
VistA Imaging is an FDA-approved Image Management system used in the Department of Veterans Affairs healthcare facilities nationwide. It is one of the most widely used image management systems in routine healthcare use, and is used to manage many different varieties of images associated with a...
System which provides a comprehensive multimedia data from many specialties, including cardiology, radiology and orthopedics. A graphical user interface
Graphical user interface
In computing, a graphical user interface is a type of user interface that allows users to interact with electronic devices with images rather than text commands. GUIs can be used in computers, hand-held devices such as MP3 players, portable media players or gaming devices, household appliances and...
known as the Computerized Patient Record System (CPRS) allows health care providers to review and update a patient’s electronic medical record at any of the VA's over 1,000 healthcare facilities. CPRS includes the ability to place orders, including medications, special procedures, X-rays, patient care nursing orders, diets, and laboratory tests.
The 2003 National Defense Authorization Act (NDAA) ensured that the VA and DoD would work together to establish a bidirectional exchange of reference quality medical images. Initially, demonstrations were only worked in El Paso, Texas, but capabilities have been expanded to six different locations of VA and DoD facilities. These facilities include VA polytrauma centers in Tampa and Richmond, Denver, North Chicago, Biloxi, and the National Capitol Area medical facilities. Radiological images such as CT scans, MRIs, and x-rays are being shared using the BHIE. Goals of the VA and DoD in the near future are to use several image sharing solutions (VistA Imaging and DoD Picture Archiving & Communications System (PACS) solutions).
Clinical Data Repository/Health Data Repository (CDHR)is a program that allows for sharing of patient records, especially allergy and pharmaceutical information, between the Department of Veteran Affairs (VA) and the Department of Defense (DoD) in the United States. The program shares data by translating the various vocabularies of the information being transmitted, allowing all of the VA facilities to access and interpret the patient records. The Laboratory Data Sharing and Interoperability (LDSI) application is a new program being implemented to allow sharing at certain sites between the VA and DoD of “chemistry and hematology laboratory tests.” Unlike the CHDR, the LDSI is currently limited in its scope.
One attribute for the start of implementing EHRs in the States is the development of the Nationwide Health Information Network which is a work in progress and still being developed. This started with the North Carolina
Healthcare Information and Communication Alliance founded in 1994 and who received funding from Department of Health and Human Services.
The Department of Veterans Affairs and Kaiser Permanente
Kaiser Permanente
Kaiser Permanente is an integrated managed care consortium, based in Oakland, California, United States, founded in 1945 by industrialist Henry J. Kaiser and physician Sidney Garfield...
has a pilot program to share health records between their systems VistA and HealthConnect, respectively.
This software called 'CONNECT' uses Nationwide Health Information Network standards and governance to make sure that health information exchanges are compatible with other exchanges being set up throughout the country. CONNECT is an open source software solution that supports electronic health information exchange. The CONNECT initiative is a Federal Health Architecture project that was conceived in 2007 and initially built by 20 various federal agencies and now comprises more than 500 organizations including federal agencies, states, healthcare providers, insurers, and health IT vendors.
The US Indian Health Service uses an EHR similar to VistA called RPMS. VistA Imaging is also being used to integrate images and co-ordinate PACS into the EHR system.
UK
As of 2005, the National Health ServiceNational Health Service
The National Health Service is the shared name of three of the four publicly funded healthcare systems in the United Kingdom. They provide a comprehensive range of health services, the vast majority of which are free at the point of use to residents of the United Kingdom...
(NHS) in the United Kingdom
United Kingdom
The United Kingdom of Great Britain and Northern IrelandIn the United Kingdom and Dependencies, other languages have been officially recognised as legitimate autochthonous languages under the European Charter for Regional or Minority Languages...
also began an EHR system. The goal of the NHS is to have 60,000,000 patients with a centralized electronic health record by 2010. The plan involves a gradual roll-out commencing May 2006, providing general practitioners in England access to the National Programme for IT (NPfIT). However, the plan has been greatly delayed and frequently criticised. As an overarching program it was stopped in 2011, although significant elements are regarded as successful and further sub-projects may continue.
Australia
AustraliaAustralia
Australia , officially the Commonwealth of Australia, is a country in the Southern Hemisphere comprising the mainland of the Australian continent, the island of Tasmania, and numerous smaller islands in the Indian and Pacific Oceans. It is the world's sixth-largest country by total area...
is dedicated to the development of a lifetime electronic health record for all its citizens. HealthConnect
HealthConnect
HealthConnect has been Australia’s change management strategy to transition from paper-based and legacy digital health records towards electronic health records planned system of electronic health records....
is the major national EHR initiative in Australia, and is made up of territory, state, and federal governments. MediConnect is a related program that provides an electronic medication record to keep track of patient prescriptions and provide stakeholders with drug alerts to avoid errors in prescribing.
Canada
The Canadian province of AlbertaAlberta
Alberta is a province of Canada. It had an estimated population of 3.7 million in 2010 making it the most populous of Canada's three prairie provinces...
started a large-scale operational EHR system project in 2005 called Alberta Netcare
Alberta Netcare
Alberta Netcare is the province of Alberta's public Electronic Health Record.-Users:There are three main categories of Netcare users:* Health service providers * Diagnostic laboratories...
, which is expected to encompass all of Alberta by 2008.
Estonia
Estonia is the first country in the world that has implemented a nationwide EHR system, registering virtually all residents' medical history from birth to death.UAE
Abu Dhabi is leading the way in using national EHR data as a live longitudinal cohort in the assessment of risk of cardiovascular disease.Saudi Arabia
Arab Health Awards 2010 recognizes Saudi Arabia National Guard Health Affairs for greatest advancement in EHR development.See also
- eMixEMixeMix, which stands for Electronic Medical Information Exchange, is a cloud computing-based technology for secure sharing of medical imaging studies and reports between disparate healthcare facilities and physicians...
- European Institute for Health RecordsEuropean Institute for Health RecordsThe European Institute for Health Records or EuroRec Institute is a non-profit organization founded in 2002 as part of the ProRec initiative. On 13 May 2003, the institute was established as a non-profit organization under French law. Current President of EuroRec is Prof. Georges De Moor...
(EuroRec) - Health informaticsHealth informatics.Health informatics is a discipline at the intersection of information science, computer science, and health care...
- Health information managementHealth Information ManagementHealth information management is the practice of maintenance and care of health records by traditional and electronic means in hospitals, physician's office clinics, health departments, health insurance companies, and other facilities that provide health care or maintenance of health records...
- List of open source healthcare software
External links
- Can Electronic Health Record Systems Transform Health Care?
- Health Information Technology in the United States
- How to Enable Standard-Compliant Streaming of Images in Electronic Health Records a white paper by Aware Inc.
- Open-Source EHR Systems for Ambulatory Care: A Market Assessment(California HealthCare Foundation, January 2008)
- US Department of Health and Human Services (HHS), Office of the National Coordinator for Health Information Technology (ONC)
- US Department of Health and Human Services (HHS), Agency for Healthcare Research and Quality (AHRQ), National Resource Center for Health Information Technology
- ICMCC portal: EHR info and blogs
- Security Aspects in Electronic Personal Health Record: Data Access and Preservation - a briefing paper at Digital Preservation EuropeDigital Preservation EuropeDigitalPreservationEurope is a European Union research project aimed at digital preservation coordination and dissemination activities within Europe. It was founded by the Sixth Framework Programme . DPE ranks among EU "Digital Libraries" priority called "i2010".DPE together with CASPAR and...

