
Senning procedure
Encyclopedia
Senning procedure is a surgical technique named after its inventor, the Swedish cardiac surgeon Åke Senning
(1915–2000), also known for implanting the first permanent cardiac pacemaker
in 1958.
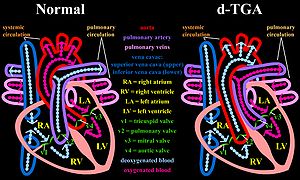
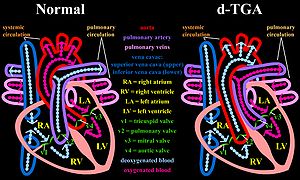
) before improvements in cardiopulmonary bypass allowed more curative surgical techniques to be feasible. In this common congenital heart defect, the venous circulation drains into the right ventricle but from this chamber, blood is directed towards the systemic circulation through the aorta. This is also expressed by the term ventriculoarterial discordance, that is the ventricles are connected to the wrong great artery (the right ventricle to the aorta, thus pumping blood from the systemic venous back into the systemic arterial circulation).
Thus, d-TGA is not to be confused with l-TGA
, where there is both atrioventricular and ventriculoarterial discordance.
 In absence of a shunt, patients with d-TGA could not survive, because there would be no flow of oxygenated blood (coming form the pulmonary veins) to the rest of the body after the normal prenatal shunts physiologically close a few weeks after birth.
In absence of a shunt, patients with d-TGA could not survive, because there would be no flow of oxygenated blood (coming form the pulmonary veins) to the rest of the body after the normal prenatal shunts physiologically close a few weeks after birth.
Before this technique became available, in 1950, two cardiac surgeons, Blalock and Hanlon, had developed a palliative procedure which consisted in opening the atrial septum. Being that in TGA the atrial septum prevents oxygenated blood from reaching the systemic circulation, this simpler procedure leads to improvements in systemic arterial O2 saturation.
In the Senning's operation, atrial tissue is used to create the baffle. No prosthetic material is introduced. A complex work of incising and refolding of the native atrial tissue is necessary to build the venous baffle. Indeed the Senning technique is technically demanding and was not widely embraced.
In 1964, Mustard described an alternative technique, the Mustard procedure
, in which the atrial septum is excised, and the atrial baffle is created by the placement of a single elephant trunk-shaped patch made of pericardial tissue. This technique has become the standard operation for TGA as it is technically less demanding.
is the preferred surgical corrective method. In this technique, the great arteries are excised and reimplanted to the corresponding ventricles. The Brazilian surgeon Jetene performed the first procedure in 1975. The coronary arteries are also explanted from the anatomical aorta, which lies on the venous side and reattached to the systemic great vessel. Indeed, the initial difficulties that prevented an earlier adoption of this approach were mostly the inability to transfer the coronary arteries, besides inadequate early techniques of cardiopulmonary bypass that precluded safe cardiac surgery in early infancy.
Long term studies have disclosed that although from the functional capacity (NYHA Class) standpoint the Senning and the Mustard operation are similar, there is a higher risk of sinus node disease and arrhythmias with the latter. Overall, in most studies the survival is good into the second decade post procedure. 78% of patients were alive after 16 years in a large follow up study from the Netherlands.
Before the utilization of surgical repair, Kirklin reports that the mortality associated with unrepaired TGA was 55%, 85%, and 90% mortality rates at 1 month, 6 months, and 1 year, respectively. This numbers correspond to all types of TGA A major factor affecting long term morbidity and mortality is the coexistence of a ventricular septal defect
(VSD). Patients with concomitant VSD may have developed also pulmonary vascular disease.
Åke Senning
Åke Senning was a pioneering Swedish cardiac surgeon, who implanted the first human implantable cardiac pacemaker in 1958, invented the Senning operation, and contributed to many other advances....
(1915–2000), also known for implanting the first permanent cardiac pacemaker
Artificial pacemaker
A pacemaker is a medical device that uses electrical impulses, delivered by electrodes contacting the heart muscles, to regulate the beating of the heart...
in 1958.
Brief History
This procedure, a form of atrial switch, was developed and first performed by Senning in 1957 as a treatment for d-TGA (dextro-Transposition of the great arteriesDextro-Transposition of the great arteries
dextro-Transposition of the great arteries , sometimes also referred to as complete transposition of the great arteries, is a birth defect in the large arteries of the heart...
) before improvements in cardiopulmonary bypass allowed more curative surgical techniques to be feasible. In this common congenital heart defect, the venous circulation drains into the right ventricle but from this chamber, blood is directed towards the systemic circulation through the aorta. This is also expressed by the term ventriculoarterial discordance, that is the ventricles are connected to the wrong great artery (the right ventricle to the aorta, thus pumping blood from the systemic venous back into the systemic arterial circulation).
Thus, d-TGA is not to be confused with l-TGA
Levo-Transposition of the great arteries
levo-Transposition of the great arteries , also commonly referred to as congenitally corrected transposition of the great arteries , is an acyanotic congenital heart defect in which the primary arteries are transposed, with the aorta anterior and to...
, where there is both atrioventricular and ventriculoarterial discordance.
Before this technique became available, in 1950, two cardiac surgeons, Blalock and Hanlon, had developed a palliative procedure which consisted in opening the atrial septum. Being that in TGA the atrial septum prevents oxygenated blood from reaching the systemic circulation, this simpler procedure leads to improvements in systemic arterial O2 saturation.
Technical aspects
With the Senning surgical repair, a baffle – or conduit - is created within the atria that reroutes the deoxygenated blood coming from the inferior and superior venae cavae to the mitral valve. This is accomplished by creating a systemic venous conduit channeling blood from the superior and inferior vena cava towards the mitral valve. After this complex plastic reconstruction using flaps from the right atrial flap, the interatrial septal flap and lets the oxygenated pulmonary venous blood flow to the tricuspid valve. The anatomic left ventricle continues to pump into the pulmonary circulation and the anatomic right ventricle will work as the systemic pump.In the Senning's operation, atrial tissue is used to create the baffle. No prosthetic material is introduced. A complex work of incising and refolding of the native atrial tissue is necessary to build the venous baffle. Indeed the Senning technique is technically demanding and was not widely embraced.
In 1964, Mustard described an alternative technique, the Mustard procedure
Mustard procedure
The Mustard procedure was developed in 1963 by Dr. William Mustard at the Hospital for Sick Children in Toronto, Canada.Dr. Mustard, with support from the Heart and Stroke Foundation of Canada, developed the first operation to correct a congenital heart defect that produced “blue babies”. The...
, in which the atrial septum is excised, and the atrial baffle is created by the placement of a single elephant trunk-shaped patch made of pericardial tissue. This technique has become the standard operation for TGA as it is technically less demanding.
Alternative surgical techniques
Currently, the arterial switch or Jatene procedureJatene procedure
The Jatene procedure, or arterial switch, is an open heart surgical procedure used to correct dextro-transposition of the great arteries ; its development was pioneered by Canadian cardiac surgeon William Mustard and it was named for Brazilian cardiac surgeon Adib Jatene, who was the first to use...
is the preferred surgical corrective method. In this technique, the great arteries are excised and reimplanted to the corresponding ventricles. The Brazilian surgeon Jetene performed the first procedure in 1975. The coronary arteries are also explanted from the anatomical aorta, which lies on the venous side and reattached to the systemic great vessel. Indeed, the initial difficulties that prevented an earlier adoption of this approach were mostly the inability to transfer the coronary arteries, besides inadequate early techniques of cardiopulmonary bypass that precluded safe cardiac surgery in early infancy.
In hospital Mortality
The acute mortality associated with the Senning procedure is reported around 5-10%. Patient selection and complexity of the congenital malformation are determinants of mortality risk.Late sequelae of the Senning procedure
Patients who have undergone such surgical correction of the congenital transposition are exposed to long term risks of cardiovascular events. In particular sinus node dysfunction, atrial arrhythmias, ventricular arrhythmias including sudden cardiac arrhythmic death, heart failure due to anatomically right ventricular failure or venous obstruction at the level of the baffle or caval anatomy have been described.Long term studies have disclosed that although from the functional capacity (NYHA Class) standpoint the Senning and the Mustard operation are similar, there is a higher risk of sinus node disease and arrhythmias with the latter. Overall, in most studies the survival is good into the second decade post procedure. 78% of patients were alive after 16 years in a large follow up study from the Netherlands.
Before the utilization of surgical repair, Kirklin reports that the mortality associated with unrepaired TGA was 55%, 85%, and 90% mortality rates at 1 month, 6 months, and 1 year, respectively. This numbers correspond to all types of TGA A major factor affecting long term morbidity and mortality is the coexistence of a ventricular septal defect
Ventricular septal defect
A ventricular septal defect is a defect in the ventricular septum, the wall dividing the left and right ventricles of the heart.The ventricular septum consists of an inferior muscular and superior membranous portion and is extensively innervated with conducting cardiomyocytes.The membranous...
(VSD). Patients with concomitant VSD may have developed also pulmonary vascular disease.

