History and naming of human leukocyte antigens
Encyclopedia
 |
 |
| HLA-A*0201 | HLA-B*3508 |
 |
|
| HLA-DQ2.5 | HLA-DR1 |
Human leukocyte antigen
Human leukocyte antigen
The human leukocyte antigen system is the name of the major histocompatibility complex in humans. The super locus contains a large number of genes related to immune system function in humans. This group of genes resides on chromosome 6, and encodes cell-surface antigen-presenting proteins and...
s (HLA) began as a list of antigen
Antigen
An antigen is a foreign molecule that, when introduced into the body, triggers the production of an antibody by the immune system. The immune system will then kill or neutralize the antigen that is recognized as a foreign and potentially harmful invader. These invaders can be molecules such as...
s identified as a result of transplant rejection. The list, HL-A1 to HL-A15. The antigens were identified based on serotype
Serotype
Serotype or serovar refers to distinct variations within a subspecies of bacteria or viruses. These microorganisms, viruses, or cells are classified together based on their cell surface antigens...
s that developed in transplant recipients, to donor antigens that could recognize one apparent antigen were found useful. HLA are not typical antigens, like those found on surface of infectious agents. HLA antigens are alloantigens, meaning they are due to the genetic differences between individuals, allo meaning different.
A person can have 2 antigen proteins per genetic-locus (one gene from each parent). During development the immune system determines these two antigens are 'self'-antigens or (autoantigens) and turns off the destructive response. However when tissues are transferred to another person they often become alloantigens. Identified antigens can therefore be clustered, creating groups in which no more than two antigens per cluster are found in a given person. Serotype group "A" consisted HL-A1, A2, A3, A9, A10, A11. Another cluster, "B", contained A7, A8, A12, A13, A14, A15. HL-A4 antigen was found to occur on lymphoid cells. Since the "HL-Antigens" no longer belonged to a single group, they were partially renamed. For example "HL-A7" became HLA-B7
HLA-B7
HLA-B7 is an HLA-B serotype. The serotype identifies the more common HLA-B*07 gene products. B7, previously HL-A7, was one of the first 'HL-A' antigens recognized, largely because of the frequency of B*0702 in Northern and Western Europe and the United States...
and "HL-A8" became HLA-B8
HLA-B8
HLA-B8 is an HLA-B serotype. The serotype identifies the HLA-B*08 gene products. HLA-B8, previously known as HL-A8 was one of the first identified of the HLA antigens. It coined the "Super B8" haplotype, also called the ancestral European haplotype because of its common occurrence in Europe,...
.
In this arrangement there were cells that were 'blank' or had new specificities
Specificity
Specificity may refer to:* Being specific * Specificity , the proportion of negatives in a binary classification test which are correctly identified...
, these new antigens were called "W" antigens, and as they were reassigned to new groups, for example "A" serotypes, they became Aw or Bw antigens. It was found that some antigens that behaved like A and B antigens but could be excluded based on '2-type max' exclusion. Thus a new group, "C" was created. Classification of C
HLA-C
HLA-C belongs to the MHC class I heavy chain receptors. The C receptor is a heterodimer consisting of a HLA-C mature gene product and β2-microglobulin. The mature C chain is anchored in the membrane...
antigens is still ongoing, and they have retained the name Cw as many serotypes have not been developed.
The classification of the "A4" antigens was complicated. The "A4" subset evolved to become D-region antigens, which was a large cluster of genes that encoded MHC class II. Several renamings occurred. The D-region has 8 major coding loci that combine to form 3 different protein groups; DP, DQ, and DR. DRw antigens were the first to be split, a process made easy by the virtue of having an invariant alpha chain, but complicated by 4 beta chain loci (DRB1, DRB3, DRB4, and DRB5). Serotypes to DQ reacted with alpha and beta chains, or both of certain isoforms. The proper classification was greatly aided by gene sequencing and PCR. Classification and description of DP antigens is ongoing.
Genetic complexity typifies HLA
The naming of human leukocyte antigens HLA "antigenAntigen
An antigen is a foreign molecule that, when introduced into the body, triggers the production of an antibody by the immune system. The immune system will then kill or neutralize the antigen that is recognized as a foreign and potentially harmful invader. These invaders can be molecules such as...
s" is deeply rooted in the discovery history of their serotype
Serotype
Serotype or serovar refers to distinct variations within a subspecies of bacteria or viruses. These microorganisms, viruses, or cells are classified together based on their cell surface antigens...
s and allele
Allele
An allele is one of two or more forms of a gene or a genetic locus . "Allel" is an abbreviation of allelomorph. Sometimes, different alleles can result in different observable phenotypic traits, such as different pigmentation...
s. There is no doubt that HLA terminology can be bewildering, this terminology is a consequence of the complex genetics as well as the way these antigens were characterized.
Historical perspective is important to an understanding how the HLA were systematized. In organ transplant the goal was to explain graft rejection for recipients, and of course, to prevent future rejection. From this perspective, the cause of rejections were found to be "antigens". In the same way bacterial antigens can cause inflammatory response, HLA antigens from the donor of the organ caused an inflammatory response when placed in a recipient. This is called allograft [allo = different, graft(medical) = transplant] rejection.
To explain rejection in a nutshell, certain immune system components are highly variable, the agents are called the Major histocompatibility (MHC) antigens. MHC antigens cause rejection of improperly matched organ transplants. The variability stems from genetics. From the perspective of human evolution, why are antigens of the MHC so variable when many other human proteins lack variability? The cause of host-versus-graft-disease may actually stem from the functions of the system.
The use of the word alloantigen actually masks the fact that HLA are infrequently autoantigens in the donor, and therefore their function is not as antigens, but something else. But the naming of these antigens is not borne out of function but the need to match organ donors with recipients.
Transplantation and transplant rejection
White blood cell
White blood cells, or leukocytes , are cells of the immune system involved in defending the body against both infectious disease and foreign materials. Five different and diverse types of leukocytes exist, but they are all produced and derived from a multipotent cell in the bone marrow known as a...
or kidney donations from other donors (called allografts, meaning 'of different genetics' grafts). If these allografts were rejected, it was found that the 'rejection' response was accompanied by an antibody
Antibody
An antibody, also known as an immunoglobulin, is a large Y-shaped protein used by the immune system to identify and neutralize foreign objects such as bacteria and viruses. The antibody recognizes a unique part of the foreign target, termed an antigen...
mediated agglutination (biology)
Agglutination (biology)
Agglutination is the clumping of particles. The word agglutination comes from the Latin agglutinare, meaning "to glue."This occurs in biology in three main examples:...
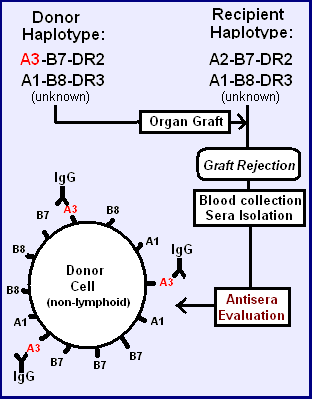
of red blood cells (See figure). The search for these cell surface antigens began. There are several processes by which antibodies can reduce function:
- Acute rejection - Antibodies could attract lymphocytes and cause them to lyse cells via the immune system's classical complement pathwayClassical complement pathwayThe Classical pathway of activation of the complement system is a group of blood proteins that mediate the specific antibody response. The main activators of the Classical Pathway are antigen-antibody complexes.-Initiation:...
- Antibodies could bind to and alter function (e.g., flow of a fluid, or prevention of binding of ligands to receptors)
- CytokineCytokineCytokines are small cell-signaling protein molecules that are secreted by the glial cells of the nervous system and by numerous cells of the immune system and are a category of signaling molecules used extensively in intercellular communication...
responses that cause systemic responses.
Different antigens can be identified
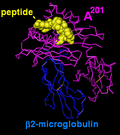
In the accompanying figure, two similar haplotypeHaplotype
A haplotype in genetics is a combination of alleles at adjacent locations on the chromosome that are transmitted together...
s (unknown to early clinicians) are identical, except for the one antigen in the top haplotype. The transplant may not be rejected, but if rejection does occur that allotypic protein, the alloantigen
Antigen
An antigen is a foreign molecule that, when introduced into the body, triggers the production of an antibody by the immune system. The immune system will then kill or neutralize the antigen that is recognized as a foreign and potentially harmful invader. These invaders can be molecules such as...
, in the donor tissue may have induced the dominant allo-reactive antibody in the recipient.
Assaying antiserum

Plasma cell
Plasma cells, also called plasma B cells, plasmocytes, and effector B cells, are white blood cells which produce large volumes of antibodies. They are transported by the blood plasma and the lymphatic system...
producing IgG. Graft recipients who generate an immune response have both IgM and IgG. The IgM can be used directly in hemagglutination
Hemagglutination
Hemagglutination, or haemagglutination, is a specific form of agglutination that involves red blood cells . It has two common uses in the laboratory: blood typing and the quantification of virus dilutions.-Blood Typing:...
assays, depicted on the right. IgM has 10 antigen binding regions per molecule, allowing cross-linking of cells. An antiserum specific for HLA-A3 will then agglutinate HLA-A3 bearing red blood cells if the concentration of IgM in the antiserum is sufficiently high. Alternatively, a second antibody to the invariable (Fc) region of the IgG can be used to cross-link antibodies on different cells, causing agglutination.
Complement fixation assay. The complement fixation test was modified to assay Antiserum mediated RBC lysis.
Chromium release assay. This assay measures the release of (biological) radioactive chromium from cells as a result of killer cell activity. These cells are attracted to class I antigens that either carry foreign antigens, or are foreign to the immune system.
The role of haplotypes in identifying antigens
| Haplotype 1 | Haplotype 2 | |||||
| Example 1 | A | Cw | B | A | Cw | B |
|---|---|---|---|---|---|---|
| Donor | 1 | 7 | 8 | 3 | 7 | 7 |
| Recipient | 1 | 7 | 8 | 2 | 7 | 7 |
| Alloreactivity | 3 | |||||
| Example 2 | ||||||
| Donor | 1 | 7 | 8 | 2 | 7 | 8 |
| Recipient | 1 | 7 | 8 | 3 | 7 | 8 |
| Alloreactivity | 2 | |||||
Each person has two HLA haplotype
Haplotype
A haplotype in genetics is a combination of alleles at adjacent locations on the chromosome that are transmitted together...
s, a cassette of genes passed on from each parent. The haplotype frequencies in Europeans are in strong linkage disequilibrium
Linkage disequilibrium
In population genetics, linkage disequilibrium is the non-random association of alleles at two or more loci, not necessarily on the same chromosome. It is also referred to as to as gametic phase disequilibrium , or simply gametic disequilibrium...
. This means there are much higher frequencies of certain haplotypes relative to the expectation based on random sorting of gene-alleles. This aided the discovery of HLA antigens, but was unknown to the pioneering researchers.
In the tables a fortuitous transplant between two unrelated individual has resulted in an antiserum to single alloantigen. By discovering these close-but-non-identical matches, the process with somewhat related haplotypes surface antigens were identified for HLA A, and in the table below, HLA B at the time however these were all grouped together as HL-Antigens. On the left the "B" and "cw" antigens are matched (B and C are close together so if B matches then C likely also matches), but A antigens are not matched. The antisera that is produced by the recipient is most likely to be A3, but if the direction of transplant is reversed A2 is the likely alloantigen. Two of the first three alloantigens are thus readily easy to detect because of the similarity and frequency of the A2-B7 and A3-B7 haplotypes.
| Haplotype 1 | Haplotype 2 | |||||
| Example 3 | A | Cw | B | A | Cw | B |
| Donor | 1 | 7 | 8 | 1 | 7 | 7 |
| Recipient | 1 | 7 | 8 | 1 | 7 | 8 |
| Alloreactivity | 7 | |||||
| Example 4 | ||||||
| Donor | 3 | 7 | 7 | 1 | 7 | 8 |
| Recipient | 3 | 7 | 7 | 1 | 7 | 7 |
| Alloreactivity | 8 | |||||
In these instances, the A1/A2, A2/A3, A1/A3 are matched, decreasing the probability of a rejection because many are linked to a given haplotype. Occasionally the 'recombinant' A1-Cw7-B7(rare), B7 becomes the alloantigen in a recipient with A1-Cw7-B8(common).
This linkage disequilibrium in Europeans explains why A1, A2, A3, "A7"[B7], and "A8"[B8] were identified, first. It would have taken substantially longer to identify other alleles because frequencies were lower, and haplotypes that migrated into the European population had undergone equilibration or were from multiple sources.
This is the genetic background against which scientists tried to uncover and understand the histocompatibility antigens.
A list of antigens created
In the late 1960s, scientist began reacting seraBlood serum
In blood, the serum is the component that is neither a blood cell nor a clotting factor; it is the blood plasma with the fibrinogens removed...
from patients with rejecting transplants to donor or 'third party' tissues. Their sera
Sera
Sera may refer to:- Music :* Sera, a Symphonic rock/electronica singer/composer/producer* Sera, the well known bass player in Greece- Places :* Sera, Hiroshima, a town in Japan* Sera District, Hiroshima, a district located in Hiroshima, Japan...
(the liquid part of the blood when blood clots) was sensitized to the cells from donors - it was alloreactive. By testing different anti-sera from recipients they were able to uncover some with unique reactivities. As a result, scientists were able to identify a few antigens. At first the first antigens were called the Hu-1 antigens and tentatively tagged as gene products of the Human equivalent of the mouse histocompatibility locus (H2). In 1968, it was discovered that matching these antigens between kidney donor and recipient improved the likelihood of kidney survival in the recipient. The antigen list still exists, although it has been reorganized to fit what we have since learned about genetics, refined, and greatly expanded.
Lymphocyte bearing antigens recognized
As the study of these 'rejection' sera
Sera
Sera may refer to:- Music :* Sera, a Symphonic rock/electronica singer/composer/producer* Sera, the well known bass player in Greece- Places :* Sera, Hiroshima, a town in Japan* Sera District, Hiroshima, a district located in Hiroshima, Japan...
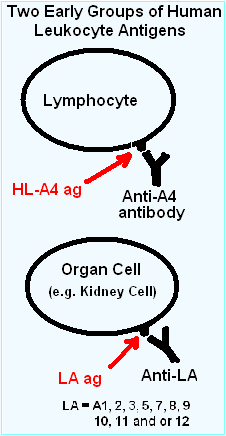
and "allo"-antigens progressed, certain patterns in the antibody recognition were recognized. The first major observation, in 1969, was that an allotypic antibodies to "4" ("Four") was only found on lymphocytes, while most of the antigens, termed "LA", recognized most cells in the body.
This group "4" antigen on lymphocytes would expand into "4a", "4b" and so on, becoming the "D" series (HLA-D (Class II) antigens) DP, DQ, and DR. This is an interesting history in itself.
The Hu-1 antigens were renamed the Human-lymphoid (HL) allo-antigens (HL-As). Allo-antigen comes from the observation that a tolerated protein in the donor becomes antigenic in the recipient. This can be compared with an autoantigen, in which a person develops antibodies to one or more of their own proteins. This also suggested the donor and recipient have a different genetic makeup for these antigens. The "LA" group thereafter was composed of HL-A1, A2, A3, A5, A6, A7, A8, A9, A10, A11, A12, A13, A14 and A15 until further divisions and renaming were necessary. Some of the antigens above, for example HL-A1, are similar to HLA-A1
HLA-A1
HLA-A1 is a human leukocyte antigen serotype within HLA-A "A" serotype group. The serotype is determined by the antibody recognition of α1 subset of HLA-A α-chains. For A1, the alpha "A" chain are encoded by the HLA-A*01 allele group and the β-chain are encoded by B2M locus. This group...
, as they are the same serotype. Some of the above, like A5, are not mentioned within the last few years, as they have been renamed.
During these early studies it became known that there were associations with many autoimmune diseases. And the HLA A1-B8 haplotype
HLA A1-B8 haplotype
HLA A1-B8 is a multigene haplotype that covers the MHC Class I region of the human major histocompatibility complex on chromosome 6...
is linked to a very long piece of conserved chromosome 6 variant called AH8.1 haplotype
HLA A1-B8-DR3-DQ2
HLA A1-B8-DR3-DQ2 haplotype is a multigene haplotype that covers a majority of the human major histocompatibility complex on chromosome 6...
. In these studies HL-A1,8 were frequently found co-linked to disease. This linkage is not necessarily a function of either gene, but a consequence of the way AH8.1 evolved.
Subclassification of lymphoid antigens

A series of tests on cultured cells revealed that, within the "LA" group, a donor tissue might have some antigens but not others. For example, an antiserum may react with patterns (on a given tissue):
- A1, A2, A7, A12
- A1, A3, A7, A8
- A1, A11, A8, A5
- A1, A8
But fail to react in the following patterns:
- A1, A2, A3, ...
- A1, A2, A11, ....
- A2, A3, A11, ....
- . . . A7, A8, A12
Series "A"
EWLINE
|
If 2 members of the series (A1, 2, 3, 9, 10, 11) were typed, a reaction with a third member of the series to the donor was not observed. This 'exclusivity' identified series "A". One might notice the similarities of this numeric series with the HLA-A series, as series "A" antigens are the first six members of HLA-A
HLA-A
HLA-A are a group of human leukocyte antigens that are encoded by the HLA-A locus on human chromosome 6p. The HLA genes constitute a large subset of the Major histocompatibility complex of humans. HLA-A is a component of certain MHC class I cell surface receptor isoforms that resides on the...
. Inadvertently, the scientist had discovered an antibody set that recognized only gene product
Gene product
A gene product is the biochemical material, either RNA or protein, resulting from expression of a gene. A measurement of the amount of gene product is sometimes used to infer how active a gene is. Abnormal amounts of gene product can be correlated with disease-causing alleles, such as the...
s from one locus, HLA-A gene the "antigens" being the gene products. The implication is that an alloreactive anti-sera can be a tool for genetic identification.
Series "B"
Not long after the series A antigens were separated from the (rapidly expanding) list of antigens, it was determined another group also could be separated along the same logical lines. This group included HL-A5, A7, A8, A12. This became the series "B".Note the similarity of Series "B" to the first few members HLA-B serotypes. The names of these antigens were necessarily changed to fit the new putative series they were assigned to. From HL-A# to HLA-B#. The problem was that the literature was using "A7" and would soon be using "B7" as short hand for HLA-B7
HLA-B7
HLA-B7 is an HLA-B serotype. The serotype identifies the more common HLA-B*07 gene products. B7, previously HL-A7, was one of the first 'HL-A' antigens recognized, largely because of the frequency of B*0702 in Northern and Western Europe and the United States...
.
Pseudo-series "w"
Since it was now certain, by the early 1970s, that the "antigens" were encoded by different series, implicit loci, numeric lists became somewhat cumbersome. Many groups were discovering antigens. In these instances an antigen was assigned a temporary name, like "RoMa2" and after discussion, the next open numeric slot could be assigned, but not to an "A" or "B" series until proper testing had been done. To work around this problem a 'workshop' number "w#" was often assigned while testing continued to determined which series the antigen belonged to.Series "C"
Before too long, a series "C" was uncovered. Series C has proved difficult to serotype, and the alleles in the series still carry the "w" tag signifying that status; in addition, it reminds us that Series C were not assigned names the same way as Series A and B, it has its own numeric list Cw1, Cw2, Cw3.Serotype group expansion and refinement
By the mid 1970s, genetic research was finally beginning to make sense of the simple list of antigens, a new series "C" had been discovered and, in turn genetic research had determined the order of HLA-A, C, B and D encoding loci on the human 6p. With new series came new antigens; Cw1 and 2 were quickly populated, although Cw typing lagged. Almost half of the antigens could not be resolved by serotyping in the early 90s. Currently genetics defines 18 groups.At this point, Dw was still being used to identify DR, DQ, and DP antigens. The ability to identify new antigens far exceeded the ability to characterize those new antigens.
As technology for transplantation was deployed around the world, it became clear that these antigens were far from a complete set, and in fact hardly useful in some areas of the world (e.g., Africa, or those descended from Africans). Some serotyping antibodies proved to be poor, with broad specificities, and new serotypes were found that identified a smaller set of antigens more precisely. These broad antigen groups, like A9 and B5, were subdivided into "split" antigen groups, A23 & A24 and B51 & B52, respectively. As the HL-A serotyping developed, so did identification of new antigens.
Genetic identification
In the early 1980s, it was discovered that a restriction fragment segregates with individuals who bear the HLA-B8HLA-B8
HLA-B8 is an HLA-B serotype. The serotype identifies the HLA-B*08 gene products. HLA-B8, previously known as HL-A8 was one of the first identified of the HLA antigens. It coined the "Super B8" haplotype, also called the ancestral European haplotype because of its common occurrence in Europe,...
serotype. By 1990, it was discovered that a single amino acid sequence difference between HLA-B44 (B*4401 versus B*4402) could result in allograft rejection. This revelation appeared to make serotyping based matching strategies problematic if many such differences existed. In the case of B44, the antigen had already been split from the B12 broad antigen group. In 1983, the cDNA sequences of HLA-A3
HLA-A3
HLA-A3 is a human leukocyte antigen serotype within HLA-A serotype group. The serotype is determined by the antibody recognition of α3 subset of HLA-A α-chains. For A3, the alpha, "A", chain are encoded by the HLA-A*03 allele group and the β-chain are encoded by B2M locus. This group currently is...
and Cw3 All three sequences compared well with mouse MHC class I antigens. The Western European HLA-B7
HLA-B7
HLA-B7 is an HLA-B serotype. The serotype identifies the more common HLA-B*07 gene products. B7, previously HL-A7, was one of the first 'HL-A' antigens recognized, largely because of the frequency of B*0702 in Northern and Western Europe and the United States...
antigen had been sequenced (although the first sequence had errors and was replaced). In short order, many HLA class I alleles were sequenced
including 2 Cw1 alleles.
By 1990, the full complexity of the HLA class I antigens was beginning to be understood. At the time new serotypes were being determined, the problem with multiple alleles for each serotype was becoming apparent by nucleotide sequencing. RFLP analysis helped determine new alleles, but sequencing was more thorough. Throughout the 1990s, PCR kits, called SSP-PCR kits were developed that allowed, at least under optimal conditions, the purification of DNA, PCR and Agarose Gel identification of alleles within an 8 hour day. Alleles that could not be clearly identified by serotype and PCR could be sequenced, allowing for the refinement of new PCR kits.
Serotypes like B*4401, B*4402, B*4403, each abundant within those with B44 serotypes could be determined with unambiguous accuracy. The molecular genetics has advanced HLA technology markedly over serotyping technology, but serotyping still survives. Serotyping had identified the most similar antigens that now form the HLA subgroups. Serotyping can reveal whether an antigen coded by the relevant HLA gene is expressed. An HLA allele coding non-expressed gene is termed "Null Allele", for example: HLA-B*15:01:01:02N. The expression level can also detected by serotyping, an HLA gene coding for antigens which has low protein expression on the cell surface is termed "Low Rxpresser", for example: HLA-A*02:01:01:02L.
Summary
- Lymphoid "antigens" became an experimental artifactIatrogenesisIatrogenesis, or an iatrogenic artifact is an inadvertent adverse effect or complication resulting from medical treatment or advice, including that of psychologists, therapists, pharmacists, nurses, physicians and dentists...
of medical techniques (i.e., of transplantation). Simply, as scientist gained familiarity with the human immune system they learned more about graft rejection, the cause was antibody production to proteins in donor tissue. The key word is allo - which means of different origin. 'Allo'typic proteins in 'allo'grafts developed immune responses in recipients. What makes these proteins different?
- From a more modern perspective, HLA gene productGene productA gene product is the biochemical material, either RNA or protein, resulting from expression of a gene. A measurement of the amount of gene product is sometimes used to infer how active a gene is. Abnormal amounts of gene product can be correlated with disease-causing alleles, such as the...
s (i.e., antigen-presenting, cell-surface receptors) did not evolve to be transplantation antigens, nor to interfere with transplantation, organ transplantation being unknown until 1960. The HLA genes are much older. Variation in HLA major antigens is the cause of transplant rejection, but variation at HLA is under preservative selection (Called heterozygous selection or balancing selectionBalancing selectionBalancing selection refers to a number of selective processes by which multiple alleles are actively maintained in the gene pool of a population at frequencies above that of gene mutation. This usually happens when the heterozygotes for the alleles under consideration have a higher adaptive value...
). Variation of HLA has led to an estimate that they are at least 60 million years in age for humans (DRB1). In humans, the number of HLA alleles is expanding, even with many genes, many more are still tolerable as immune presentation antigens.
The scientific problem has been to explain the natural function of a molecule, such as a self cell-surface receptor involved in immunity
Immunity (medical)
Immunity is a biological term that describes a state of having sufficient biological defenses to avoid infection, disease, or other unwanted biological invasion. Immunity involves both specific and non-specific components. The non-specific components act either as barriers or as eliminators of wide...
. It also seeks to explain how variation developed (perhaps by evolutionary pressure), and how the genetic mechanisms works (dominant, codominant, semidominant, or recessive
Recessive
In genetics, the term "recessive gene" refers to an allele that causes a phenotype that is only seen in a homozygous genotype and never in a heterozygous genotype. Every person has two copies of every gene on autosomal chromosomes, one from mother and one from father...
; purifying selection or balancing selection
Balancing selection
Balancing selection refers to a number of selective processes by which multiple alleles are actively maintained in the gene pool of a population at frequencies above that of gene mutation. This usually happens when the heterozygotes for the alleles under consideration have a higher adaptive value...
).

