
Atypical trigeminal neuralgia
Encyclopedia
Atypical Trigeminal Neuralgia (ATN), or Type 2 Trigeminal Neuralgia, is a rare form of Trigeminal neuralgia
, a disorder of the fifth cranial nerve. This form of neuralgia
is difficult to diagnose, as it is rare and the symptoms overlap with several other disorders. The symptoms can occur in addition to having migraine headache, or be mistaken for migraine alone, or dental problems such as Temporomandibular joint disorder
, musculoskeletal issues, and hypochondriasis. ATN can have a wide range of symptoms and the pain
can fluctuate in intensity from mild aching to a crushing or burning sensation, and also to the extreme pain experienced with the more common trigeminal neuralgia.
Many TN and ATN patients have pain that is "triggered" by light touch on shifting trigger zones. ATN pain tends to worsen with talking, smiling, chewing, or in response to sensations such as a cool breeze. The pain from ATN is often continuous, and periods of remission are rare. Both TN and ATN can be bilateral, though the character of pain is usually different on the two sides at any one time.
 ATN is usually attributed to inflammation or demyelination, with increased sensitivity of the trigeminal nerve
ATN is usually attributed to inflammation or demyelination, with increased sensitivity of the trigeminal nerve
. These effects are believed to be caused by dental procedures, infection, demyelinating diseases, or compression of the trigeminal nerve (by an impinging vein or artery, a tumor, or arterio-veinous malformation). An interesting aspect is that this form affects both men and women equally and can occur at any age, unlike typical trigeminal neuralgia, which is seen most commonly in women. Though TN and ATN most often present in the fifth decade, cases have been documented as early as infancy.
ATN often goes undiagnosed or misdiagnosed for extended periods, leading to a great deal of unexplained pain and anxiety. A National Patient Survey conducted by the US Trigeminal Neuralgia Association in the late 1990s indicated that the average facial neuralgia patient may see six different physicians before receiving a first definitive diagnosis. The first practitioner to see facial neuralgia patients is often a dentist who may lack deep training in facial neurology. Thus ATN may be mis-diagnosed as Tempormandibular Joint Disorder.
This disorder is regarded by many medical professionals to comprise the most severe form of chronic pain known in medical practice. In some patients, pain may be unresponsive even to opioid drugs at any dose level that leaves the patient conscious. The disorder has thus acquired the unfortunate and possibly inflammatory nickname, "the suicide disease".
Symptoms of ATN may overlap those of a dental problem called "Atypical Odontalgia" [literal meaning "unusual tooth pain"], with aching, burning, or stabs of pain localized to one or more teeth and adjacent jaw. The pain may seem to shift from one tooth to the next, after root canals or extractions. In desperate efforts to alleviate pain, some patients undergo multiple (but unneeded) root canals or extractions, even in the absence of suggestive X-ray evidence of dental abscess.
ATN symptoms may also be similar to those of Post Herpetic Neuralgia, which causes nerve inflammation when the latent Herpes Zoster virus of a previous case of Chicken Pox re-emerges in Shingles. Fortunately, Post-Herpetic Neuralgia is generally treated with medications which are also effective against ATN.
The subject of atypical trigeminal neuralgia is considered problematic even among experts. Some forms of orofacial pain are relatively well defined and easy to recognize while the others seem to represent a diverse group of pain syndromes with considerable overlap, several classification schemes, vague characterization and controversial entities. The term Atypical TN is broad and due to the complexity of the condition, there are considerable issues with defining the condition further. Some medical practitioners no longer make a distinction between facial neuralgia (a nominal condition of inflammation) versus facial neuropathy (direct physical damage to a nerve).
Due to the variability and imprecision of their pain symptoms, ATN or Atypical Odontalgia patients may be misdiagnosed with "Atypical Facial Pain
" or "Hypocondriasis", both of which are considered problematic by many practitioners. The term "Atypical Facial Pain
" is sometimes assigned to pain which crosses the mid-line of the face or otherwise does not conform to expected boundaries of nerve distributions or characteristics of validated medical entities. As such, the term is seen to comprise a diagnosis by reduction.
As noted in material published by the [US] National Pain Foundation: "Atypical Facial Pain
is a confusing term and should never be used to describe patients with trigeminal neuralgia or trigeminal neuropathic pain. Strictly speaking, AFP is classified as a “somatiform pain disorder”; this is a psychological diagnosis that should be confirmed by a skilled pain psychologist. Patients with the diagnosis of AFP have no identifiable underlying physical cause for the pain. The pain is usually constant, described as aching or burning, and often affects both sides of the face (this is almost never the case in patients with trigeminal neuralgia). The pain frequently involves areas of the head, face, and neck that are outside the sensory territories that are supplied by the trigeminal nerve. It is important to correctly identify patients with AFP since the treatment for this is strictly medical. Surgical procedures are not indicated for Atypical Facial Pain
."
The term "Hypochondriosis" is closely related to "Somatiform Pain Disorder" and "Conversion Disorder" in the Diagnostic and Statistical Manual (DSM-IV) of the American Psychiatric Association. As of July 2011, this axis of the DSM-IV is undergoing major revision for the DSM-V, with introduction of a new designation "Complex Somatic Symptom Disorder". However, it remains to be demonstrated that any of these "disorders" can reliably be diagnosed as a medical entity with a discrete and reliable course of therapy.
It is possible that there are triggers or aggravating factors that patients need to learn to recognize to help manage their health. Bright lights, sounds, stress, and poor diet are examples of additional stimuli that can contribute to the condition. The pain can cause nausea, so beyond the obvious need to treat the pain, it is important to be sure to try to get adequate rest and nutrition.
Depression is frequently co-morbid with neuralgia and neuropathic pain of all sorts, as a result of the negative effects that pain has on one's life. Depression and chronic pain may interact, with chronic pain often predisposing patients to depression, and depression operating to sap energy, disrupt sleep and heighten sensitivity and the sense of suffering. Dealing with depression should thus be considered equally important as finding direct relief from the pain.
If the anti-seizure drugs are found ineffective, the supervising physician may introduce one of the tri-cyclic anti-depressant medications such as Amitriptyline (Elavil) or Nortriptyline (Pamelor), among others. The tri-cyclic antidepressants are known to have dual action against both depression and neuropathic pain. Other drugs which may also be tried, either individually or in combination with an anti-seizure agent, include Baclofen, Lyrica, tranquilizers, muscle relaxants, and opioid drugs such as Percocet or Oxycodone.
For some ATN patients, treatment with opioid drugs may represent the only viable medical option which preserves quality of life and personal functioning. Although there is considerable controversy in public policy and practice in this branch of medicine, practice guidelines have long been available and published.
If drug treatment is found to be ineffective or causes disabling side effects for the patient, one of several neurosurgical procedures may be considered. The available procedures are believed to be less effective with Type II (Atypical) Trigeminal Neuralgia than with Type I (Typical or "classic") TN. Among present procedures, the most effective and long lasting has been found to be Micro-Vascular Decompression (MVD), which seeks to relieve direct compression of the Trigeminal Nerve by separating and padding blood vessels in the vicinity of the emergence of this nerve from the brain stem, below the cranium. Radio Frequency Rhizotomy has similar outcome statistics, with a different mechanism. Rhizotomy introduces a controlled lesion on the nerve distribution further downstream from the brain stem, to interrupt or moderate nerve response and over-sensitivity. Less effective forms of Rhizotomy include Balloon Compression and Glycerol Rhizotomy. Radiosurgery (Gamma radiation or electron beam) techniques — Gamma Knife or Cyber Knife — require no surgical incision. However initial results and persistence of results are not as good as for MVD or RF Rhizotomy.
Choice of a surgical procedure is made by the doctor and patient in consultation, based on the patient's pain presentation and health and the doctor's medical experience. Some neurosurgeons resist the application of MVD or other surgeries to Atypical Trigeminal Neuralgia, in light of a wide spread perception that ATN pain is less responsive to these procedures. However, recent papers suggest that in cases where pain initially presents as Type I TN, surgery may be effective even after the pain has evolved into Type II.
Trigeminal neuralgia
Trigeminal neuralgia , tic douloureux is a neuropathic disorder characterized by episodes of intense pain in the face, originating from the trigeminal nerve. It has been described as among the most painful conditions known...
, a disorder of the fifth cranial nerve. This form of neuralgia
Neuralgia
Neuralgia is pain in one or more nerves that occurs without stimulation of pain receptor cells. Neuralgia pain is produced by a change in neurological structure or function rather than by the excitation of pain receptors that causes nociceptive pain. Neuralgia falls into two categories: central...
is difficult to diagnose, as it is rare and the symptoms overlap with several other disorders. The symptoms can occur in addition to having migraine headache, or be mistaken for migraine alone, or dental problems such as Temporomandibular joint disorder
Temporomandibular joint disorder
Temporomandibular joint disorder , or TMJ syndrome, is an umbrella term covering acute or chronic inflammation of the temporomandibular joint, which connects the mandible to the skull. The disorder and resultant dysfunction can result in significant pain and impairment...
, musculoskeletal issues, and hypochondriasis. ATN can have a wide range of symptoms and the pain
Pain
Pain is an unpleasant sensation often caused by intense or damaging stimuli such as stubbing a toe, burning a finger, putting iodine on a cut, and bumping the "funny bone."...
can fluctuate in intensity from mild aching to a crushing or burning sensation, and also to the extreme pain experienced with the more common trigeminal neuralgia.
Symptoms
ATN pain can be described as heavy, aching, stabbing and burning. Some sufferers have a constant migraine-like headache. Others may experience intense pain in one or in all three trigeminal nerve branches, including teeth, ears, sinuses, cheeks, forehead, upper and lower jaws, "behind" the eyes, and scalp. In addition, those with ATN may also experience the shocks or stabs found in type 1 TN.Many TN and ATN patients have pain that is "triggered" by light touch on shifting trigger zones. ATN pain tends to worsen with talking, smiling, chewing, or in response to sensations such as a cool breeze. The pain from ATN is often continuous, and periods of remission are rare. Both TN and ATN can be bilateral, though the character of pain is usually different on the two sides at any one time.
Causes
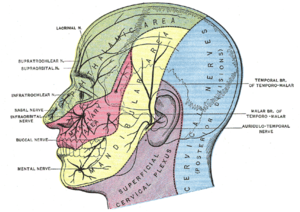
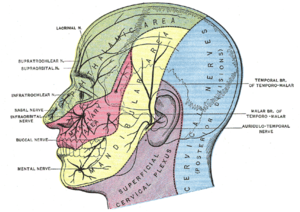
Trigeminal nerve
The trigeminal nerve contains both sensory and motor fibres. It is responsible for sensation in the face and certain motor functions such as biting, chewing, and swallowing. Sensory information from the face and body is processed by parallel pathways in the central nervous system...
. These effects are believed to be caused by dental procedures, infection, demyelinating diseases, or compression of the trigeminal nerve (by an impinging vein or artery, a tumor, or arterio-veinous malformation). An interesting aspect is that this form affects both men and women equally and can occur at any age, unlike typical trigeminal neuralgia, which is seen most commonly in women. Though TN and ATN most often present in the fifth decade, cases have been documented as early as infancy.
Risks
Both forms of Facial Neuralgia are relatively rare, with an incidence recently estimated between 12 and 24 new cases per hundred thousand population per year.ATN often goes undiagnosed or misdiagnosed for extended periods, leading to a great deal of unexplained pain and anxiety. A National Patient Survey conducted by the US Trigeminal Neuralgia Association in the late 1990s indicated that the average facial neuralgia patient may see six different physicians before receiving a first definitive diagnosis. The first practitioner to see facial neuralgia patients is often a dentist who may lack deep training in facial neurology. Thus ATN may be mis-diagnosed as Tempormandibular Joint Disorder.
This disorder is regarded by many medical professionals to comprise the most severe form of chronic pain known in medical practice. In some patients, pain may be unresponsive even to opioid drugs at any dose level that leaves the patient conscious. The disorder has thus acquired the unfortunate and possibly inflammatory nickname, "the suicide disease".
Symptoms of ATN may overlap those of a dental problem called "Atypical Odontalgia" [literal meaning "unusual tooth pain"], with aching, burning, or stabs of pain localized to one or more teeth and adjacent jaw. The pain may seem to shift from one tooth to the next, after root canals or extractions. In desperate efforts to alleviate pain, some patients undergo multiple (but unneeded) root canals or extractions, even in the absence of suggestive X-ray evidence of dental abscess.
ATN symptoms may also be similar to those of Post Herpetic Neuralgia, which causes nerve inflammation when the latent Herpes Zoster virus of a previous case of Chicken Pox re-emerges in Shingles. Fortunately, Post-Herpetic Neuralgia is generally treated with medications which are also effective against ATN.
The subject of atypical trigeminal neuralgia is considered problematic even among experts. Some forms of orofacial pain are relatively well defined and easy to recognize while the others seem to represent a diverse group of pain syndromes with considerable overlap, several classification schemes, vague characterization and controversial entities. The term Atypical TN is broad and due to the complexity of the condition, there are considerable issues with defining the condition further. Some medical practitioners no longer make a distinction between facial neuralgia (a nominal condition of inflammation) versus facial neuropathy (direct physical damage to a nerve).
Due to the variability and imprecision of their pain symptoms, ATN or Atypical Odontalgia patients may be misdiagnosed with "Atypical Facial Pain
Atypical facial pain
Atypical Facial Pain has historically been regarded as a pathological condition, including a wide group of facial pain problems. Generally, this pain is neuropathic in presentation, consisting of burning, superficial or deep-aching, stabbing pain. AFP may also be described as poorly localized,...
" or "Hypocondriasis", both of which are considered problematic by many practitioners. The term "Atypical Facial Pain
Atypical facial pain
Atypical Facial Pain has historically been regarded as a pathological condition, including a wide group of facial pain problems. Generally, this pain is neuropathic in presentation, consisting of burning, superficial or deep-aching, stabbing pain. AFP may also be described as poorly localized,...
" is sometimes assigned to pain which crosses the mid-line of the face or otherwise does not conform to expected boundaries of nerve distributions or characteristics of validated medical entities. As such, the term is seen to comprise a diagnosis by reduction.
As noted in material published by the [US] National Pain Foundation: "Atypical Facial Pain
Atypical facial pain
Atypical Facial Pain has historically been regarded as a pathological condition, including a wide group of facial pain problems. Generally, this pain is neuropathic in presentation, consisting of burning, superficial or deep-aching, stabbing pain. AFP may also be described as poorly localized,...
is a confusing term and should never be used to describe patients with trigeminal neuralgia or trigeminal neuropathic pain. Strictly speaking, AFP is classified as a “somatiform pain disorder”; this is a psychological diagnosis that should be confirmed by a skilled pain psychologist. Patients with the diagnosis of AFP have no identifiable underlying physical cause for the pain. The pain is usually constant, described as aching or burning, and often affects both sides of the face (this is almost never the case in patients with trigeminal neuralgia). The pain frequently involves areas of the head, face, and neck that are outside the sensory territories that are supplied by the trigeminal nerve. It is important to correctly identify patients with AFP since the treatment for this is strictly medical. Surgical procedures are not indicated for Atypical Facial Pain
Atypical facial pain
Atypical Facial Pain has historically been regarded as a pathological condition, including a wide group of facial pain problems. Generally, this pain is neuropathic in presentation, consisting of burning, superficial or deep-aching, stabbing pain. AFP may also be described as poorly localized,...
."
The term "Hypochondriosis" is closely related to "Somatiform Pain Disorder" and "Conversion Disorder" in the Diagnostic and Statistical Manual (DSM-IV) of the American Psychiatric Association. As of July 2011, this axis of the DSM-IV is undergoing major revision for the DSM-V, with introduction of a new designation "Complex Somatic Symptom Disorder". However, it remains to be demonstrated that any of these "disorders" can reliably be diagnosed as a medical entity with a discrete and reliable course of therapy.
It is possible that there are triggers or aggravating factors that patients need to learn to recognize to help manage their health. Bright lights, sounds, stress, and poor diet are examples of additional stimuli that can contribute to the condition. The pain can cause nausea, so beyond the obvious need to treat the pain, it is important to be sure to try to get adequate rest and nutrition.
Depression is frequently co-morbid with neuralgia and neuropathic pain of all sorts, as a result of the negative effects that pain has on one's life. Depression and chronic pain may interact, with chronic pain often predisposing patients to depression, and depression operating to sap energy, disrupt sleep and heighten sensitivity and the sense of suffering. Dealing with depression should thus be considered equally important as finding direct relief from the pain.
Treatment
Treatment of patients believed to have ATN or TN is usually begun with medication. The long-time first drug of choice for facial neuralgia has been Carbamazepine (Tegretol), an anti-seizure agent. Due to the significant side-effects and hazards of this drug, others have recently come into common use as alternatives. These include Oxcarbazepine (Trileptal), Lamotrigine (Lamictal), and Gabapentin (Neurontin). A positive patient response to one of these medications might be considered as supporting evidence for the diagnosis, which is otherwise made from medical history and pain presentation. There are no present medical tests to conclusively confirm TN or ATN.If the anti-seizure drugs are found ineffective, the supervising physician may introduce one of the tri-cyclic anti-depressant medications such as Amitriptyline (Elavil) or Nortriptyline (Pamelor), among others. The tri-cyclic antidepressants are known to have dual action against both depression and neuropathic pain. Other drugs which may also be tried, either individually or in combination with an anti-seizure agent, include Baclofen, Lyrica, tranquilizers, muscle relaxants, and opioid drugs such as Percocet or Oxycodone.
For some ATN patients, treatment with opioid drugs may represent the only viable medical option which preserves quality of life and personal functioning. Although there is considerable controversy in public policy and practice in this branch of medicine, practice guidelines have long been available and published.
If drug treatment is found to be ineffective or causes disabling side effects for the patient, one of several neurosurgical procedures may be considered. The available procedures are believed to be less effective with Type II (Atypical) Trigeminal Neuralgia than with Type I (Typical or "classic") TN. Among present procedures, the most effective and long lasting has been found to be Micro-Vascular Decompression (MVD), which seeks to relieve direct compression of the Trigeminal Nerve by separating and padding blood vessels in the vicinity of the emergence of this nerve from the brain stem, below the cranium. Radio Frequency Rhizotomy has similar outcome statistics, with a different mechanism. Rhizotomy introduces a controlled lesion on the nerve distribution further downstream from the brain stem, to interrupt or moderate nerve response and over-sensitivity. Less effective forms of Rhizotomy include Balloon Compression and Glycerol Rhizotomy. Radiosurgery (Gamma radiation or electron beam) techniques — Gamma Knife or Cyber Knife — require no surgical incision. However initial results and persistence of results are not as good as for MVD or RF Rhizotomy.
Choice of a surgical procedure is made by the doctor and patient in consultation, based on the patient's pain presentation and health and the doctor's medical experience. Some neurosurgeons resist the application of MVD or other surgeries to Atypical Trigeminal Neuralgia, in light of a wide spread perception that ATN pain is less responsive to these procedures. However, recent papers suggest that in cases where pain initially presents as Type I TN, surgery may be effective even after the pain has evolved into Type II.
External links
- Trigeminal Neuralgia Fact Sheet National Institute of Neurological Disorders and Stroke

