
Platelet
Encyclopedia
Platelets, or thrombocytes (from Greek θρόμβος, "clot" and κύτος, "cell"), are small,
irregularly shaped clear cell fragments (i.e. cells that do not have a nucleus
containing DNA), 2–3 µm in diameter, which are derived from fragmentation of precursor megakaryocyte
s. The average lifespan of a platelet is normally just 5 to 9 days. Platelets are a natural source of growth factors. They circulate in the blood
of mammal
s and are involved in hemostasis
, leading to the formation of blood clots
.
If the number of platelets is too low, excessive bleeding can occur. However, if the number of platelets is too high, blood clots can form (thrombosis
), which may obstruct blood vessels and result in such events as a stroke
, myocardial infarction
, pulmonary embolism
or the blockage of blood vessels to other parts of the body, such as the extremities of the arms or legs. An abnormality or disease of the platelets is called a thrombocytopathy, which could be either a low number of platelets (thrombocytopenia
), a decrease in function of platelets (thrombasthenia), or an increase in the number of platelets (thrombocytosis
). There are disorders that reduce the number of platelets, such as heparin-induced thrombocytopenia
(HIT) or thrombotic thrombocytopenic purpura
(TTP) that typically cause thromboses, or clots, instead of bleeding.
Platelets release a multitude of growth factors including Platelet-derived growth factor
(PDGF), a potent chemotactic
agent, and TGF beta
, which stimulates the deposition of extracellular matrix
. Both of these growth factors have been shown to play a significant role in the repair and regeneration of connective tissue
s. Other healing-associated growth factors produced by platelets include basic fibroblast growth factor
, insulin-like growth factor 1
, platelet-derived epidermal growth factor
, and vascular endothelial growth factor
. Local application of these factors in increased concentrations through Platelet-rich plasma
(PRP) has been used as an adjunct to wound healing
for several decades.
. This is achieved primarily by the formation of thrombi, when damage to the endothelium
of blood vessel
s occurs. On the converse, thrombus formation must be inhibited at times when there is no damage to the endothelium.
, endothelial-ADPase, and PGI2
. Endothelial-ADPase clears away the platelet activator, ADP
.
Endothelial cells produce a protein called von Willebrand factor
(vWF), a cell adhesion ligand
, which helps endothelial cells adherne to collagen
in the basement membrane
. Under physiological conditions, collagen is not exposed to the bloodstream. vWF is secreted constitutively into the plasma
by the endothelial cells, and is stored in granules within the endothelial cell and in platelets.
When the endothelial layer is injured, collagen
, vWF and tissue factor
from the subendothelium is exposed to the bloodstream. When the platelets contact collagen or vWF, they are activated (e.g. to clump together). They are also activated by thrombin
(formed with the help of tissue factor). They can also be activated by a negatively-charged surface, such as glass.
Platelet activation further results in the scramblase
-mediated transport of negatively-charged phospholipid
s to the platelet surface. These phospholipids provide a catalytic surface (with the charge provided by phosphatidylserine
and phosphatidylethanolamine
) for the tenase
and prothrombinase
complexes. Calcium ions are essential for binding of these coagulation factors.
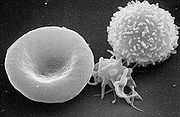 Activated platelets change in shape to become more spherical, and pseudopods form on their surface. Thus they assume a stellate shape.
Activated platelets change in shape to become more spherical, and pseudopods form on their surface. Thus they assume a stellate shape.
and dense granule
s. Activated platelets excrete the contents of these granules into their canalicular systems and into surrounding blood. There are three types of granules:
pathway to produce TXA2
. TXA2 is involved in activating other platelets and its formation is inhibited by COX
inhibitors, such as aspirin
.
and von Willebrand factor
(vWF) as a connecting agent. The most abundant platelet aggregation receptor is glycoprotein IIb/IIIa
(gpIIb/IIIa); this is a calcium-dependent receptor for fibrinogen, fibronectin
, vitronectin
, thrombospondin
, and vWF. Other receptors include GPIb-V-IX complex (vWF) and GPVI
(collagen
).
Activated platelets will adhere, via glycoprotein
(GP) Ia, to the collagen that is exposed by endothelial damage. Aggregation and adhesion act together to form the platelet plug. Myosin
and actin
filaments in platelets are stimulated to contract during aggregation, further reinforcing the plug.
Platelet aggregation is stimulated by ADP
, thromboxane
, and α2 receptor-activation, but inhibited by other inflammatory products like PGI2 and PGD2. Platelet aggregation is enhanced by exogenous administration of anabolic steroids.
, and the platelets are cleared by phagocytosis.
(1) and P2Y(12). Although abnormalities in all three genes have been documented clinical correlation is available only for P2Y(12). Patients with P2Y(12) defects have a mild to moderate bleeding diathesis, characterized by mucocutaneous bleedings and excessive post-surgical and post-traumatic blood loss. A defects in P2Y(12) should be suspected when ADP
, even at concentrations ≥10 micro molar, is unable to induce full, irreversible platelet aggregation. Confirmation of the diagnosis is with tests that evaluate the degree of inhibition of adenylyl cyclase by ADP.
, platelets are rapidly deployed to sites of injury or infection, and potentially modulate inflammatory processes by interacting with leukocytes and by secreting cytokines, chemokines, and other inflammatory mediators. Platelets also secrete platelet-derived growth factor
(PDGF).
). Ninety-five percent of healthy people will have platelet counts in this range. Some will have statistically abnormal platelet counts while having no demonstrable abnormality. However, if it is either very low or very high, the likelihood of an abnormality being present is higher.
Both thrombocytopenia
and thrombocytosis
may present with coagulation problems. In general, low platelet counts increase bleeding risks; however there are exceptions (such as immune-mediated heparin-induced thrombocytopenia
or paroxysmal nocturnal hemoglobinuria
). High counts may lead to thrombosis, although this is mainly when the elevated count is due to myeloproliferative disorder.
Transfusion is generally used only to correct unusually low platelet counts (typically below (1.0–1.5)×1010/L). Transfusion is contraindicated in thrombotic thrombocytopenic purpura
(TTP), as it fuels the coagulopathy
. In patients undergoing surgery
, a level below 5×1010/L is associated with abnormal surgical bleeding, and regional anaesthetic procedures such as epidural
s are avoided for levels below 80–100.
Normal platelet counts are not a guarantee of adequate function. In some states, the platelets, while being adequate in number, are dysfunctional. For instance, aspirin
irreversibly disrupts platelet function by inhibiting cyclooxygenase
-1 (COX1), and hence normal hemostasis. The resulting platelets are unable to produce new cyclooxygenase because they have no DNA. Normal platelet function will not return until the use of aspirin has ceased and enough of the affected platelets have been replaced by new ones, which can take over a week. Ibuprofen
, another NSAID, does not have such a long duration effect, with platelet function usually returning within 24 hours, and taking ibuprofen before aspirin will prevent the irreversible effects of aspirin. Uremia
, a consequence of renal failure
, leads to platelet dysfunction that may be ameliorated by the administration of desmopressin
.
, clopidogrel
, cilostazol, ticlopidine
, and prasugrel
.
Intravenous agents often used to alter/suppress platelet function include: abciximab, eptifibatide
, tirofiban
.
In addition to platelet transfusion, hematopoetic agents such as Oprelvekin
, Romiplostim
, and Eltrombopag
can be used to increase platelet counts.
Alloimmune disorders
Disorders leading to platelet dysfunction or reduced count:
Disorders featuring an elevated count:
Disorders of platelet adhesion or aggregation:
Disorders of platelet metabolism
Disorders that indirectly compromise platelet function:
Disorders in which platelets play a key role:
(1632–1723), it was the German anatomist Max Schultze (1825–1874) who first offered a description of the platelet in his newly founded journal Archiv für mikroscopische Anatomie. He describes "spherules" to be much smaller than red blood cells that are occasionally clumped and may participate in collections of fibrous material
. He recommends further study of the findings.
Giulio Bizzozero
(1846–1901), building on Schultze's findings, used "living circulation" to study blood cells of amphibians microscopically in vivo
. He is especially noted for discovering that platelets clump at the site of blood vessel injury, a process that precedes the formation of a blood clot
. This observation confirmed the role of platelets in coagulation
.
 Platelets are either isolated from collected units of whole blood
Platelets are either isolated from collected units of whole blood
and pooled to make a therapeutic dose or collected by apheresis
, sometimes concurrently with plasma
or red blood cells. The industry standard is for platelets to be tested for bacteria
before transfusion to avoid septic reactions, which can be fatal. Recently the AABB Industry Standards for Blood Banks and Transfusion Services (5.1.5.1) has allowed for use of pathogen reduction technology as an alternative to bacterial screenings in platelets.
Pooled whole-blood platelets, sometimes called "random" platelets, are made primarily by two methods. In the US, a unit of whole blood is placed into a large centrifuge
in what is referred to as a "soft spin." At these settings, the platelets remain suspended in the plasma. The platelet-rich plasma (PRP) is removed from the RBCs, then centrifuged at a faster setting to harvest the platelets from the plasma. In other regions of the world, the unit of whole blood is centrifuged using settings that cause the platelets to become suspended in the "buffy coat" layer, which includes the platelets and the white blood cells. The "buffy coat" is isolated in a sterile bag, suspended in a small amount of red blood cells and plasma, then centrifuged again to separate the platelets and plasma from the red and white blood cells. Regardless of the initial method of preparation, multiple platelets may be combined into one container using a sterile connection device to manufacture a single product with the desired therapeutic dose.
Apheresis platelets are collected using a mechanical device that draws blood from the donor and centrifuges the collected blood to separate out the platelets and other components to be collected. The remaining blood is returned to the donor. The advantage to this method is that a single donation provides at least one therapeutic dose, as opposed to the multiple donations for whole-blood platelets. This means that a recipient is not exposed to as many different donors and has less risk of transfusion-transmitted disease and other complications. Sometimes a person such as a cancer
patient that requires routine transfusions of platelets will receive repeated donations from a specific donor to further minimize the risk. Pathogen reduction of platelets using for example, riboflavin and UV light treatments
can also be carried out to reduce the infectious load of pathogens contained in donated blood products, thereby reducing the risk of transmission of transfusion transmitted diseases.
Platelets are not cross-matched unless they contain a significant amount of red blood cell
s (RBCs), which results in a reddish-orange color to the product. This is usually associated with whole-blood platelets, as apheresis methods are more efficient than "soft spin" centrifugation at isolating the specific components of blood. An effort is usually made to issue type specific platelets, but this is not as critical as it is with RBCs.
Platelets collected by either method have a very short shelf life, typically five days. This results in frequent problems with short supply, as testing the donations often requires up to a full day. Since there are no effective preservative solutions for platelets, they lose potency quickly and are best when fresh.
Platelets are stored under constant agitation at 20–24 °C. Storage at room temperature provides an environment where any bacteria that are introduced to the blood component during the collection process may proliferate and subsequently cause bacteremia in the patient. Regulations are in place in the United States that require products to be tested for the presence of bacterial contamination before transfusion.
Platelets, either apheresis or random-donor platelets, can be processed through a volume reduction process. In this process, the platelets are spun in a centrifuge and the excess plasma is removed, leaving 10 to 100 mL of platelet concentrate. Volume-reduced platelets are normally transfused only to neonatal and pediatric patients when a large volume of plasma could overload the child's small circulatory system. The lower volume of plasma also reduces the chances of an adverse transfusion reaction to plasma proteins. Volume reduced platelets have a shelf life of only four hours.
irregularly shaped clear cell fragments (i.e. cells that do not have a nucleus
Cell nucleus
In cell biology, the nucleus is a membrane-enclosed organelle found in eukaryotic cells. It contains most of the cell's genetic material, organized as multiple long linear DNA molecules in complex with a large variety of proteins, such as histones, to form chromosomes. The genes within these...
containing DNA), 2–3 µm in diameter, which are derived from fragmentation of precursor megakaryocyte
Megakaryocyte
The megakaryocyte is a bone marrow cell responsible for the production of blood thrombocytes , which are necessary for normal blood clotting...
s. The average lifespan of a platelet is normally just 5 to 9 days. Platelets are a natural source of growth factors. They circulate in the blood
Blood
Blood is a specialized bodily fluid in animals that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells....
of mammal
Mammal
Mammals are members of a class of air-breathing vertebrate animals characterised by the possession of endothermy, hair, three middle ear bones, and mammary glands functional in mothers with young...
s and are involved in hemostasis
Hemostasis
Hemostasis or haemostasis is a process which causes bleeding to stop, meaning to keep blood within a damaged blood vessel . Most of the time this includes blood changing from a liquid to a solid state. Intact blood vessels are central to moderating blood's tendency to clot...
, leading to the formation of blood clots
Thrombus
A thrombus , or blood clot, is the final product of the blood coagulation step in hemostasis. It is achieved via the aggregation of platelets that form a platelet plug, and the activation of the humoral coagulation system...
.
If the number of platelets is too low, excessive bleeding can occur. However, if the number of platelets is too high, blood clots can form (thrombosis
Thrombosis
Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel is injured, the body uses platelets and fibrin to form a blood clot to prevent blood loss...
), which may obstruct blood vessels and result in such events as a stroke
Stroke
A stroke, previously known medically as a cerebrovascular accident , is the rapidly developing loss of brain function due to disturbance in the blood supply to the brain. This can be due to ischemia caused by blockage , or a hemorrhage...
, myocardial infarction
Myocardial infarction
Myocardial infarction or acute myocardial infarction , commonly known as a heart attack, results from the interruption of blood supply to a part of the heart, causing heart cells to die...
, pulmonary embolism
Pulmonary embolism
Pulmonary embolism is a blockage of the main artery of the lung or one of its branches by a substance that has travelled from elsewhere in the body through the bloodstream . Usually this is due to embolism of a thrombus from the deep veins in the legs, a process termed venous thromboembolism...
or the blockage of blood vessels to other parts of the body, such as the extremities of the arms or legs. An abnormality or disease of the platelets is called a thrombocytopathy, which could be either a low number of platelets (thrombocytopenia
Thrombocytopenia
Thrombocytopenia is a relative decrease of platelets in blood.A normal human platelet count ranges from 150,000 to 450,000 platelets per microliter of blood. These limits are determined by the 2.5th lower and upper percentile, so values outside this range do not necessarily indicate disease...
), a decrease in function of platelets (thrombasthenia), or an increase in the number of platelets (thrombocytosis
Thrombocytosis
Thrombocytosis is the presence of high platelet counts in the blood, and can be either primary or reactive...
). There are disorders that reduce the number of platelets, such as heparin-induced thrombocytopenia
Heparin-induced thrombocytopenia
Heparin-induced thrombocytopenia is the development of thrombocytopenia , due to the administration of various forms of heparin, an anticoagulant...
(HIT) or thrombotic thrombocytopenic purpura
Thrombotic thrombocytopenic purpura
Thrombotic thrombocytopenic purpura is a rare disorder of the blood-coagulation system, causing extensive microscopic thromboses to form in small blood vessels throughout the body...
(TTP) that typically cause thromboses, or clots, instead of bleeding.
Platelets release a multitude of growth factors including Platelet-derived growth factor
Platelet-derived growth factor
In molecular biology, platelet-derived growth factor is one of the numerous growth factors, or proteins that regulate cell growth and division. In particular, it plays a significant role in blood vessel formation , the growth of blood vessels from already-existing blood vessel tissue. Uncontrolled...
(PDGF), a potent chemotactic
Chemotaxis
Chemotaxis is the phenomenon in which somatic cells, bacteria, and other single-cell or multicellular organisms direct their movements according to certain chemicals in their environment. This is important for bacteria to find food by swimming towards the highest concentration of food molecules,...
agent, and TGF beta
TGF beta
Transforming growth factor beta is a protein that controls proliferation, cellular differentiation, and other functions in most cells. It plays a role in immunity, cancer, heart disease, diabetes, Marfan syndrome, and Loeys–Dietz syndrome....
, which stimulates the deposition of extracellular matrix
Extracellular matrix
In biology, the extracellular matrix is the extracellular part of animal tissue that usually provides structural support to the animal cells in addition to performing various other important functions. The extracellular matrix is the defining feature of connective tissue in animals.Extracellular...
. Both of these growth factors have been shown to play a significant role in the repair and regeneration of connective tissue
Connective tissue
"Connective tissue" is a fibrous tissue. It is one of the four traditional classes of tissues . Connective Tissue is found throughout the body.In fact the whole framework of the skeleton and the different specialized connective tissues from the crown of the head to the toes determine the form of...
s. Other healing-associated growth factors produced by platelets include basic fibroblast growth factor
Fibroblast growth factor
Fibroblast growth factors, or FGFs, are a family of growth factors involved in angiogenesis, wound healing, and embryonic development. The FGFs are heparin-binding proteins and interactions with cell-surface associated heparan sulfate proteoglycans have been shown to be essential for FGF signal...
, insulin-like growth factor 1
Insulin-like growth factor 1
Insulin-like growth factor 1 also known as somatomedin C is a protein that in humans is encoded by the IGF1 gene. IGF-1 has also been referred to as a "sulfation factor" and its effects were termed "nonsuppressible insulin-like activity" in the 1970s.IGF-1 is a hormone similar in molecular...
, platelet-derived epidermal growth factor
Epidermal growth factor
Epidermal growth factor or EGF is a growth factor that plays an important role in the regulation of cell growth, proliferation, and differentiation by binding to its receptor EGFR...
, and vascular endothelial growth factor
Vascular endothelial growth factor
Vascular endothelial growth factor is a signal protein produced by cells that stimulates vasculogenesis and angiogenesis. It is part of the system that restores the oxygen supply to tissues when blood circulation is inadequate....
. Local application of these factors in increased concentrations through Platelet-rich plasma
Platelet-rich plasma
Platelet-rich plasma is blood plasma that has been enriched with platelets. As a concentrated source of autologous platelets, PRP contains several different growth factors and other cytokines that stimulate healing of bone and soft tissue.-Components:The efficacy of certain growth factors in...
(PRP) has been used as an adjunct to wound healing
Wound healing
Wound healing, or cicatrisation, is an intricate process in which the skin repairs itself after injury. In normal skin, the epidermis and dermis exists in a steady-state equilibrium, forming a protective barrier against the external environment...
for several decades.
Kinetics
- Platelets are produced in blood cell formation (thrombopoiesisThrombopoiesisThrombopoiesis refers to the process of thrombocyte generation.Thromobocytes are ligations of the cytoplasm from megakaryocytes. A single megakaryocyte can give rise to thousands of thrombocytes....
) in bone marrowBone marrowBone marrow is the flexible tissue found in the interior of bones. In humans, bone marrow in large bones produces new blood cells. On average, bone marrow constitutes 4% of the total body mass of humans; in adults weighing 65 kg , bone marrow accounts for approximately 2.6 kg...
, by budding off from megakaryocytes. - The physiological range for platelets is (150–400)×109 per liter.
- Around 1011 platelets are produced each day by an average healthy adult.
- The lifespan of circulating platelets is 5 to 9 days.
- Megakaryocyte and platelet production is regulated by thrombopoietinThrombopoietinThrombopoietin also known as megakaryocyte growth and development factor is a protein that in humans is encoded by the THPO gene....
, a hormone usually produced by the liverLiverThe liver is a vital organ present in vertebrates and some other animals. It has a wide range of functions, including detoxification, protein synthesis, and production of biochemicals necessary for digestion...
and kidneyKidneyThe kidneys, organs with several functions, serve essential regulatory roles in most animals, including vertebrates and some invertebrates. They are essential in the urinary system and also serve homeostatic functions such as the regulation of electrolytes, maintenance of acid–base balance, and...
s. - Each megakaryocyteMegakaryocyteThe megakaryocyte is a bone marrow cell responsible for the production of blood thrombocytes , which are necessary for normal blood clotting...
produces between 5,000 and 10,000 platelets. - Old platelets are destroyed by phagocytosis in the spleenSpleenThe spleen is an organ found in virtually all vertebrate animals with important roles in regard to red blood cells and the immune system. In humans, it is located in the left upper quadrant of the abdomen. It removes old red blood cells and holds a reserve of blood in case of hemorrhagic shock...
and by Kupffer cellKupffer cellKupffer cells, also known as Browicz-Kupffer cells and stellate macrophages, are specialized macrophages located in the liver lining the walls of the sinusoids that form part of the reticuloendothelial system .-History:The cells were first observed by Karl Wilhelm von Kupffer in 1876...
s in the liverLiverThe liver is a vital organ present in vertebrates and some other animals. It has a wide range of functions, including detoxification, protein synthesis, and production of biochemicals necessary for digestion...
. - Reserve platelets are stored in the spleen, and are released when needed by sympathetically-induced splenic contraction.
Thrombus formation
The function of platelets is the maintenance of hemostasisHemostasis
Hemostasis or haemostasis is a process which causes bleeding to stop, meaning to keep blood within a damaged blood vessel . Most of the time this includes blood changing from a liquid to a solid state. Intact blood vessels are central to moderating blood's tendency to clot...
. This is achieved primarily by the formation of thrombi, when damage to the endothelium
Endothelium
The endothelium is the thin layer of cells that lines the interior surface of blood vessels, forming an interface between circulating blood in the lumen and the rest of the vessel wall. These cells are called endothelial cells. Endothelial cells line the entire circulatory system, from the heart...
of blood vessel
Blood vessel
The blood vessels are the part of the circulatory system that transports blood throughout the body. There are three major types of blood vessels: the arteries, which carry the blood away from the heart; the capillaries, which enable the actual exchange of water and chemicals between the blood and...
s occurs. On the converse, thrombus formation must be inhibited at times when there is no damage to the endothelium.
Activation
The inner surface of blood vessels is lined with a thin layer of endothelial cells that, in normal hemostasis, acts to inhibit platelet activation by producing nitric oxideNitric oxide
Nitric oxide, also known as nitrogen monoxide, is a diatomic molecule with chemical formula NO. It is a free radical and is an important intermediate in the chemical industry...
, endothelial-ADPase, and PGI2
Prostacyclin
Prostacyclin is a member of the family of lipid molecules known as eicosanoids.As a drug, it is also known as "epoprostenol". The terms are sometimes used interchangeably.-History:...
. Endothelial-ADPase clears away the platelet activator, ADP
Adenosine diphosphate
Adenosine diphosphate, abbreviated ADP, is a nucleoside diphosphate. It is an ester of pyrophosphoric acid with the nucleoside adenosine. ADP consists of the pyrophosphate group, the pentose sugar ribose, and the nucleobase adenine....
.
Endothelial cells produce a protein called von Willebrand factor
Von Willebrand factor
von Willebrand factor is a blood glycoprotein involved in hemostasis. It is deficient or defective in von Willebrand disease and is involved in a large number of other diseases, including thrombotic thrombocytopenic purpura, Heyde's syndrome, and possibly hemolytic-uremic syndrome...
(vWF), a cell adhesion ligand
Ligand (biochemistry)
In biochemistry and pharmacology, a ligand is a substance that forms a complex with a biomolecule to serve a biological purpose. In a narrower sense, it is a signal triggering molecule, binding to a site on a target protein.The binding occurs by intermolecular forces, such as ionic bonds, hydrogen...
, which helps endothelial cells adherne to collagen
Collagen
Collagen is a group of naturally occurring proteins found in animals, especially in the flesh and connective tissues of mammals. It is the main component of connective tissue, and is the most abundant protein in mammals, making up about 25% to 35% of the whole-body protein content...
in the basement membrane
Basement membrane
The basement membrane is a thin sheet of fibers that underlies the epithelium, which lines the cavities and surfaces of organs including skin, or the endothelium, which lines the interior surface of blood vessels.- Composition :...
. Under physiological conditions, collagen is not exposed to the bloodstream. vWF is secreted constitutively into the plasma
Blood plasma
Blood plasma is the straw-colored liquid component of blood in which the blood cells in whole blood are normally suspended. It makes up about 55% of the total blood volume. It is the intravascular fluid part of extracellular fluid...
by the endothelial cells, and is stored in granules within the endothelial cell and in platelets.
When the endothelial layer is injured, collagen
Collagen
Collagen is a group of naturally occurring proteins found in animals, especially in the flesh and connective tissues of mammals. It is the main component of connective tissue, and is the most abundant protein in mammals, making up about 25% to 35% of the whole-body protein content...
, vWF and tissue factor
Tissue factor
Tissue factor, also called platelet tissue factor, factor III, thrombokinase, or CD142 is a protein present in subendothelial tissue, platelets, and leukocytes necessary for the initiation of thrombin formation from the zymogen prothrombin. An incorrect synonym is thromboplastin...
from the subendothelium is exposed to the bloodstream. When the platelets contact collagen or vWF, they are activated (e.g. to clump together). They are also activated by thrombin
Thrombin
Thrombin is a "trypsin-like" serine protease protein that in humans is encoded by the F2 gene. Prothrombin is proteolytically cleaved to form thrombin in the first step of the coagulation cascade, which ultimately results in the stemming of blood loss...
(formed with the help of tissue factor). They can also be activated by a negatively-charged surface, such as glass.
Platelet activation further results in the scramblase
Scramblase
Scramblase is a protein responsible for the translocation of phospholipids between the two monolayers of a lipid bilayer of a cell membrane. In humans, phospholipid scramblases constitute a family of five homologous proteins that are named as hPLSCR1–hPLSCR5. Scramblases are members of the...
-mediated transport of negatively-charged phospholipid
Phospholipid
Phospholipids are a class of lipids that are a major component of all cell membranes as they can form lipid bilayers. Most phospholipids contain a diglyceride, a phosphate group, and a simple organic molecule such as choline; one exception to this rule is sphingomyelin, which is derived from...
s to the platelet surface. These phospholipids provide a catalytic surface (with the charge provided by phosphatidylserine
Phosphatidylserine
Phosphatidylserine is a phospholipid component, usually kept on the inner-leaflet of cell membranes by an enzyme called flippase...
and phosphatidylethanolamine
Phosphatidylethanolamine
Phosphatidylethanolamine is a lipid found in biological membranes. It is synthesized by the addition of CDP-ethanolamine to diglyceride, releasing CMP. S-adenosyl methionine can subsequently methylate the amine of phosphatidyl ethanolamine to yield phosphatidyl choline.Cephalin is a phospholipid,...
) for the tenase
Tenase
In coagulation, the procoagulant protein factor X can be activated into factor Xa two ways. Extrinsic and intrinsic ways.The activating complexes are called tenase...
and prothrombinase
Prothrombinase
The prothrombinase complex consists of the serine protease, Factor Xa, and the protein cofactor, Factor Va. The complex assembles on negatively charged phospholipid membranes in the presence of calcium ions. The prothrombinase complex catalyzes the conversion of prothrombin , an inactive zymogen,...
complexes. Calcium ions are essential for binding of these coagulation factors.
Shape change
Granule secretion
Platelets contain alphaPlatelet alpha-granule
In platelets, the term "alpha granules" is used to describe granules containing several growth factors.-Contents:Contents include insulin-like growth factor 1, platelet-derived growth factor, TGFβ, platelet factor 4 and other clotting proteins In platelets, the term "alpha granules" is used to...
and dense granule
Dense granule
Dense granules are specialized secretory organelles.-In unicellular organisms:They are found in animals and in unicellular organisms including Apicomplexa protozoans....
s. Activated platelets excrete the contents of these granules into their canalicular systems and into surrounding blood. There are three types of granules:
- dense (or delta) granulesDense granuleDense granules are specialized secretory organelles.-In unicellular organisms:They are found in animals and in unicellular organisms including Apicomplexa protozoans....
(containing ADPAdenosine diphosphateAdenosine diphosphate, abbreviated ADP, is a nucleoside diphosphate. It is an ester of pyrophosphoric acid with the nucleoside adenosine. ADP consists of the pyrophosphate group, the pentose sugar ribose, and the nucleobase adenine....
or ATPAdenosine triphosphateAdenosine-5'-triphosphate is a multifunctional nucleoside triphosphate used in cells as a coenzyme. It is often called the "molecular unit of currency" of intracellular energy transfer. ATP transports chemical energy within cells for metabolism...
, calciumCalciumCalcium is the chemical element with the symbol Ca and atomic number 20. It has an atomic mass of 40.078 amu. Calcium is a soft gray alkaline earth metal, and is the fifth-most-abundant element by mass in the Earth's crust...
, and serotoninSerotoninSerotonin or 5-hydroxytryptamine is a monoamine neurotransmitter. Biochemically derived from tryptophan, serotonin is primarily found in the gastrointestinal tract, platelets, and in the central nervous system of animals including humans...
) - lambda granules – similar to lysosomes and contain several hydrolytic enzymes.
- Alpha granulesPlatelet alpha-granuleIn platelets, the term "alpha granules" is used to describe granules containing several growth factors.-Contents:Contents include insulin-like growth factor 1, platelet-derived growth factor, TGFβ, platelet factor 4 and other clotting proteins In platelets, the term "alpha granules" is used to...
(containing platelet factor 4Platelet factor 4Platelet factor 4 is a small cytokine belonging to the CXC chemokine family that is also known as chemokine ligand 4 . This chemokine is released from alpha-granules of activated platelets during platelet aggregation, and promotes blood coagulation by moderating the effects of heparin-like...
, transforming growth factor-β1TGF beta 1Transforming growth factor beta 1 or TGF-β1 is a polypeptide member of the transforming growth factor beta superfamily of cytokines. It is a secreted protein that performs many cellular functions, including the control of cell growth, cell proliferation, cell differentiation and apoptosis...
, platelet-derived growth factorPlatelet-derived growth factorIn molecular biology, platelet-derived growth factor is one of the numerous growth factors, or proteins that regulate cell growth and division. In particular, it plays a significant role in blood vessel formation , the growth of blood vessels from already-existing blood vessel tissue. Uncontrolled...
, fibronectinFibronectinFibronectin is a high-molecular weight glycoprotein of the extracellular matrix that binds to membrane-spanning receptor proteins called integrins. In addition to integrins, fibronectin also binds extracellular matrix components such as collagen, fibrin and heparan sulfate proteoglycans...
, B-thromboglobulin, vWFVon Willebrand factorvon Willebrand factor is a blood glycoprotein involved in hemostasis. It is deficient or defective in von Willebrand disease and is involved in a large number of other diseases, including thrombotic thrombocytopenic purpura, Heyde's syndrome, and possibly hemolytic-uremic syndrome...
, fibrinogenFibrinogenFibrinogen is a soluble plasma glycoprotein, synthesised by the liver, that is converted by thrombin into fibrin during blood coagulation. This is achieved through processes in the coagulation cascade that activate the zymogen prothrombin to the serine protease thrombin, which is responsible for...
, and coagulation factors VFactor VFactor V is a protein of the coagulation system, rarely referred to as proaccelerin or labile factor. In contrast to most other coagulation factors, it is not enzymatically active but functions as a cofactor...
and XIIIFactor XIIIFactor XIII or fibrin stabilizing factor is an enzyme of the blood coagulation system that crosslinks fibrin.- Function :Factor XIII is a transglutaminase that circulates in the plasma as a heterotetramer of two catalytic A subunits and two carrier B subunits...
).
Thromboxane A2 synthesis
Platelet activation initiates the arachidonic acidArachidonic acid
Arachidonic acid is a polyunsaturated omega-6 fatty acid 20:4.It is the counterpart to the saturated arachidic acid found in peanut oil, Arachidonic acid (AA, sometimes ARA) is a polyunsaturated omega-6 fatty acid 20:4(ω-6).It is the counterpart to the saturated arachidic acid found in peanut oil,...
pathway to produce TXA2
Thromboxane
Thromboxane is a member of the family of lipids known as eicosanoids. The two major thromboxanes are thromboxane A2 and thromboxane B2. The distinguishing feature of thromboxanes is a 6-membered ether-containing ring....
. TXA2 is involved in activating other platelets and its formation is inhibited by COX
Cyclooxygenase
Cyclooxygenase is an enzyme that is responsible for formation of important biological mediators called prostanoids, including prostaglandins, prostacyclin and thromboxane. Pharmacological inhibition of COX can provide relief from the symptoms of inflammation and pain...
inhibitors, such as aspirin
Aspirin
Aspirin , also known as acetylsalicylic acid , is a salicylate drug, often used as an analgesic to relieve minor aches and pains, as an antipyretic to reduce fever, and as an anti-inflammatory medication. It was discovered by Arthur Eichengrun, a chemist with the German company Bayer...
.
Adhesion and aggregation
Platelets aggregate, or clump together, using fibrinogenFibrinogen
Fibrinogen is a soluble plasma glycoprotein, synthesised by the liver, that is converted by thrombin into fibrin during blood coagulation. This is achieved through processes in the coagulation cascade that activate the zymogen prothrombin to the serine protease thrombin, which is responsible for...
and von Willebrand factor
Von Willebrand factor
von Willebrand factor is a blood glycoprotein involved in hemostasis. It is deficient or defective in von Willebrand disease and is involved in a large number of other diseases, including thrombotic thrombocytopenic purpura, Heyde's syndrome, and possibly hemolytic-uremic syndrome...
(vWF) as a connecting agent. The most abundant platelet aggregation receptor is glycoprotein IIb/IIIa
Glycoprotein IIb/IIIa
In medicine, glycoprotein IIb/IIIa is an integrin complex found on platelets. It is a receptor for fibrinogen and aids in platelet activation. The complex is formed via calcium-dependent association of gpIIb and gpIIIa, a required step in normal platelet aggregation and endothelial adherence...
(gpIIb/IIIa); this is a calcium-dependent receptor for fibrinogen, fibronectin
Fibronectin
Fibronectin is a high-molecular weight glycoprotein of the extracellular matrix that binds to membrane-spanning receptor proteins called integrins. In addition to integrins, fibronectin also binds extracellular matrix components such as collagen, fibrin and heparan sulfate proteoglycans...
, vitronectin
Vitronectin
Vitronectin also known as VTN is a protein that in humans is encoded by the VTN gene.The protein encoded by this gene is a member of the pexin family...
, thrombospondin
Thrombospondin
Thrombospondins are secreted proteins with antiangiogenic abilities. TSP was discovered by Nancy L. Baenziger.-Types:The thrombospondins are a family of multifunctional proteins...
, and vWF. Other receptors include GPIb-V-IX complex (vWF) and GPVI
GPVI
Glycoprotein VI also known as GPVI is a glycoprotein receptor for collagen which is expressed in platelets. In humans, glycoprotein VI is encoded by the GPVI gene.- Function :...
(collagen
Collagen
Collagen is a group of naturally occurring proteins found in animals, especially in the flesh and connective tissues of mammals. It is the main component of connective tissue, and is the most abundant protein in mammals, making up about 25% to 35% of the whole-body protein content...
).
Activated platelets will adhere, via glycoprotein
Glycoprotein
Glycoproteins are proteins that contain oligosaccharide chains covalently attached to polypeptide side-chains. The carbohydrate is attached to the protein in a cotranslational or posttranslational modification. This process is known as glycosylation. In proteins that have segments extending...
(GP) Ia, to the collagen that is exposed by endothelial damage. Aggregation and adhesion act together to form the platelet plug. Myosin
Myosin
Myosins comprise a family of ATP-dependent motor proteins and are best known for their role in muscle contraction and their involvement in a wide range of other eukaryotic motility processes. They are responsible for actin-based motility. The term was originally used to describe a group of similar...
and actin
Actin
Actin is a globular, roughly 42-kDa moonlighting protein found in all eukaryotic cells where it may be present at concentrations of over 100 μM. It is also one of the most highly-conserved proteins, differing by no more than 20% in species as diverse as algae and humans...
filaments in platelets are stimulated to contract during aggregation, further reinforcing the plug.
Platelet aggregation is stimulated by ADP
Adenosine diphosphate
Adenosine diphosphate, abbreviated ADP, is a nucleoside diphosphate. It is an ester of pyrophosphoric acid with the nucleoside adenosine. ADP consists of the pyrophosphate group, the pentose sugar ribose, and the nucleobase adenine....
, thromboxane
Thromboxane
Thromboxane is a member of the family of lipids known as eicosanoids. The two major thromboxanes are thromboxane A2 and thromboxane B2. The distinguishing feature of thromboxanes is a 6-membered ether-containing ring....
, and α2 receptor-activation, but inhibited by other inflammatory products like PGI2 and PGD2. Platelet aggregation is enhanced by exogenous administration of anabolic steroids.
Wound repair
The blood clot is only a temporary solution to stop bleeding; vessel repair is therefore needed. The aggregated platelets help this process by secreting chemicals that promote the invasion of fibroblasts from surrounding connective tissue into the wounded area to completely heal the wound or form a scar. The obstructing clot is slowly dissolved by the fibrinolytic enzyme, plasminPlasmin
Plasmin is an important enzyme present in blood that degrades many blood plasma proteins, most notably, fibrin clots. The degradation of fibrin is termed fibrinolysis. In humans, the plasmin protein is encoded by the PLG gene.- Function :...
, and the platelets are cleared by phagocytosis.
P2 receptors
Human platelets have three types of P2 receptors: P2X(1), P2YP2Y receptor
P2Y receptors are a family of purinergic receptors, G protein-coupled receptors stimulated by nucleotides such as ATP, ADP, UTP, UDP and UDP-glucose...
(1) and P2Y(12). Although abnormalities in all three genes have been documented clinical correlation is available only for P2Y(12). Patients with P2Y(12) defects have a mild to moderate bleeding diathesis, characterized by mucocutaneous bleedings and excessive post-surgical and post-traumatic blood loss. A defects in P2Y(12) should be suspected when ADP
Adenosine diphosphate
Adenosine diphosphate, abbreviated ADP, is a nucleoside diphosphate. It is an ester of pyrophosphoric acid with the nucleoside adenosine. ADP consists of the pyrophosphate group, the pentose sugar ribose, and the nucleobase adenine....
, even at concentrations ≥10 micro molar, is unable to induce full, irreversible platelet aggregation. Confirmation of the diagnosis is with tests that evaluate the degree of inhibition of adenylyl cyclase by ADP.
Other functions
- Clot retractionClot retractionClot retraction is the "shrinking" of a blood clot over a number of days. In so doing, the edges of the blood vessel wall at the point of injury are slowly brought together again to repair the damage....
- Pro-coagulation
- InflammationInflammationInflammation is part of the complex biological response of vascular tissues to harmful stimuli, such as pathogens, damaged cells, or irritants. Inflammation is a protective attempt by the organism to remove the injurious stimuli and to initiate the healing process...
- CytokineCytokineCytokines are small cell-signaling protein molecules that are secreted by the glial cells of the nervous system and by numerous cells of the immune system and are a category of signaling molecules used extensively in intercellular communication...
signalling - Phagocytosis
Cytokine signaling
In addition to being the chief cellular effector of hemostasisHemostasis
Hemostasis or haemostasis is a process which causes bleeding to stop, meaning to keep blood within a damaged blood vessel . Most of the time this includes blood changing from a liquid to a solid state. Intact blood vessels are central to moderating blood's tendency to clot...
, platelets are rapidly deployed to sites of injury or infection, and potentially modulate inflammatory processes by interacting with leukocytes and by secreting cytokines, chemokines, and other inflammatory mediators. Platelets also secrete platelet-derived growth factor
Platelet-derived growth factor
In molecular biology, platelet-derived growth factor is one of the numerous growth factors, or proteins that regulate cell growth and division. In particular, it plays a significant role in blood vessel formation , the growth of blood vessels from already-existing blood vessel tissue. Uncontrolled...
(PDGF).
High and low counts
A normal platelet count in a healthy individual is between 150,000 and 450,000 per μl (microlitre) of blood ((150–450)×109/LLitre
pic|200px|right|thumb|One litre is equivalent to this cubeEach side is 10 cm1 litre water = 1 kilogram water The litre is a metric system unit of volume equal to 1 cubic decimetre , to 1,000 cubic centimetres , and to 1/1,000 cubic metre...
). Ninety-five percent of healthy people will have platelet counts in this range. Some will have statistically abnormal platelet counts while having no demonstrable abnormality. However, if it is either very low or very high, the likelihood of an abnormality being present is higher.
Both thrombocytopenia
Thrombocytopenia
Thrombocytopenia is a relative decrease of platelets in blood.A normal human platelet count ranges from 150,000 to 450,000 platelets per microliter of blood. These limits are determined by the 2.5th lower and upper percentile, so values outside this range do not necessarily indicate disease...
and thrombocytosis
Thrombocytosis
Thrombocytosis is the presence of high platelet counts in the blood, and can be either primary or reactive...
may present with coagulation problems. In general, low platelet counts increase bleeding risks; however there are exceptions (such as immune-mediated heparin-induced thrombocytopenia
Heparin-induced thrombocytopenia
Heparin-induced thrombocytopenia is the development of thrombocytopenia , due to the administration of various forms of heparin, an anticoagulant...
or paroxysmal nocturnal hemoglobinuria
Paroxysmal nocturnal hemoglobinuria
Paroxysmal nocturnal hemoglobinuria , sometimes referred to as Marchiafava-Micheli syndrome, is a rare, acquired, potentially life-threatening disease of the blood characterised by complement-induced intravascular hemolytic anemia , red urine and thrombosis...
). High counts may lead to thrombosis, although this is mainly when the elevated count is due to myeloproliferative disorder.
Transfusion is generally used only to correct unusually low platelet counts (typically below (1.0–1.5)×1010/L). Transfusion is contraindicated in thrombotic thrombocytopenic purpura
Thrombotic thrombocytopenic purpura
Thrombotic thrombocytopenic purpura is a rare disorder of the blood-coagulation system, causing extensive microscopic thromboses to form in small blood vessels throughout the body...
(TTP), as it fuels the coagulopathy
Coagulopathy
Coagulopathy is a condition in which the blood’s ability to clot is impaired. This condition can cause prolonged or excessive bleeding, which may occur spontaneously or following an injury or medical and dental procedures.The normal clotting process depends on the interplay of various proteins in...
. In patients undergoing surgery
Surgery
Surgery is an ancient medical specialty that uses operative manual and instrumental techniques on a patient to investigate and/or treat a pathological condition such as disease or injury, or to help improve bodily function or appearance.An act of performing surgery may be called a surgical...
, a level below 5×1010/L is associated with abnormal surgical bleeding, and regional anaesthetic procedures such as epidural
Epidural
The term epidural is often short for epidural analgesia, a form of regional analgesia involving injection of drugs through a catheter placed into the epidural space...
s are avoided for levels below 80–100.
Normal platelet counts are not a guarantee of adequate function. In some states, the platelets, while being adequate in number, are dysfunctional. For instance, aspirin
Aspirin
Aspirin , also known as acetylsalicylic acid , is a salicylate drug, often used as an analgesic to relieve minor aches and pains, as an antipyretic to reduce fever, and as an anti-inflammatory medication. It was discovered by Arthur Eichengrun, a chemist with the German company Bayer...
irreversibly disrupts platelet function by inhibiting cyclooxygenase
Cyclooxygenase
Cyclooxygenase is an enzyme that is responsible for formation of important biological mediators called prostanoids, including prostaglandins, prostacyclin and thromboxane. Pharmacological inhibition of COX can provide relief from the symptoms of inflammation and pain...
-1 (COX1), and hence normal hemostasis. The resulting platelets are unable to produce new cyclooxygenase because they have no DNA. Normal platelet function will not return until the use of aspirin has ceased and enough of the affected platelets have been replaced by new ones, which can take over a week. Ibuprofen
Ibuprofen
Ibuprofen is a nonsteroidal anti-inflammatory drug used for relief of symptoms of arthritis, fever, as an analgesic , especially where there is an inflammatory component, and dysmenorrhea....
, another NSAID, does not have such a long duration effect, with platelet function usually returning within 24 hours, and taking ibuprofen before aspirin will prevent the irreversible effects of aspirin. Uremia
Uremia
Uremia or uraemia is a term used to loosely describe the illness accompanying kidney failure , in particular the nitrogenous waste products associated with the failure of this organ....
, a consequence of renal failure
Renal failure
Renal failure or kidney failure describes a medical condition in which the kidneys fail to adequately filter toxins and waste products from the blood...
, leads to platelet dysfunction that may be ameliorated by the administration of desmopressin
Desmopressin
Desmopressin is a synthetic replacement for vasopressin, the hormone that reduces urine production. It may be taken nasally, intravenously, or as a tablet...
.
Medications
Oral agents often used to alter/suppress platelet function include aspirinAspirin
Aspirin , also known as acetylsalicylic acid , is a salicylate drug, often used as an analgesic to relieve minor aches and pains, as an antipyretic to reduce fever, and as an anti-inflammatory medication. It was discovered by Arthur Eichengrun, a chemist with the German company Bayer...
, clopidogrel
Clopidogrel
Clopidogrel is an oral, thienopyridine class antiplatelet agent used to inhibit blood clots in coronary artery disease, peripheral vascular disease, and cerebrovascular disease. It is marketed by Bristol-Myers Squibb and Sanofi-Aventis under the trade name Plavix. The drug works by irreversibly...
, cilostazol, ticlopidine
Ticlopidine
Ticlopidine is an antiplatelet drug in the thienopyridine family. Like clopidogrel, it is an adenosine diphosphate receptor inhibitor. It is used in patients in whom aspirin is not tolerated, or in whom dual antiplatelet therapy is desirable...
, and prasugrel
Prasugrel
Prasugrel is a novel platelet inhibitor developed by Daiichi Sankyo Co. and produced by Ube and currently marketed in the United States in cooperation with Eli Lilly and Company for acute coronary syndromes planned for percutaneous coronary intervention...
.
Intravenous agents often used to alter/suppress platelet function include: abciximab, eptifibatide
Eptifibatide
Eptifibatide , is an antiplatelet drug of the glycoprotein IIb/IIIa inhibitor class. Eptifibatide is a cyclic heptapeptide derived from a protein found in the venom of the southeastern pygmy rattlesnake...
, tirofiban
Tirofiban
Tirofiban is an antiplatelet drug. It belongs to a class of antiplatelet named glycoprotein IIb/IIIa inhibitors...
.
In addition to platelet transfusion, hematopoetic agents such as Oprelvekin
Oprelvekin
Oprelvekin is recombinant interleukin eleven , a thrombopoietic growth factor that directly stimulates the proliferation of hematopoietic stem cells and megakaryocyte progenitor cells and induces megakaryocyte maturation resulting in increased platelet production...
, Romiplostim
Romiplostim
Romiplostim is a fusion protein analog of thrombopoietin, a hormone that regulates platelet production. The drug was developed by Amgen and is marketed under the trade name Nplate through a restricted usage program called NEXUS...
, and Eltrombopag
Eltrombopag
Eltrombopag is a medication that has been developed for conditions that lead to thrombocytopenia . It is a small molecule agonist of the c-mpl receptor, which is the physiological target of the hormone thrombopoietin...
can be used to increase platelet counts.
Diseases
Disorders leading to a reduced platelet count:- ThrombocytopeniaThrombocytopeniaThrombocytopenia is a relative decrease of platelets in blood.A normal human platelet count ranges from 150,000 to 450,000 platelets per microliter of blood. These limits are determined by the 2.5th lower and upper percentile, so values outside this range do not necessarily indicate disease...
- Idiopathic thrombocytopenic purpuraIdiopathic thrombocytopenic purpuraIdiopathic thrombocytopenic purpura is the condition of having an abnormally low platelet count of no known cause . As most incidents of ITP appear to be related to the production of antibodies against platelets, immune thrombocytopenic purpura or immune thrombocytopenia are terms also used to...
– also known as immune thrombocytopenic purpura (ITP) - Thrombotic thrombocytopenic purpuraThrombotic thrombocytopenic purpuraThrombotic thrombocytopenic purpura is a rare disorder of the blood-coagulation system, causing extensive microscopic thromboses to form in small blood vessels throughout the body...
- Drug-induced thrombocytopenic purpuraDrug-induced thrombocytopenic purpuraDrug-induced thrombocytopenic purpura is a skin condition result from a low platelet count due to drug-induced anti-platelet antibodies caused by drugs such as heparin, sulfonamines, digoxin, quinine, and quinidine....
(for example heparin-induced thrombocytopeniaHeparin-induced thrombocytopeniaHeparin-induced thrombocytopenia is the development of thrombocytopenia , due to the administration of various forms of heparin, an anticoagulant...
(HIT))
- Idiopathic thrombocytopenic purpura
- Gaucher's diseaseGaucher's diseaseGaucher's disease is a genetic disease in which a fatty substance accumulates in cells and certain organs.Gaucher's disease is the most common of the lysosomal storage diseases. It is caused by a hereditary deficiency of the enzyme glucosylceramidase. The enzyme acts on the fatty acid...
- Aplastic anemiaAplastic anemiaAplastic anemia is a condition where bone marrow does not produce sufficient new cells to replenish blood cells. The condition, per its name, involves both aplasia and anemia...
- OnyalaiOnyalaiOnyalai is a form of thrombocytopenia that affects some of the population in areas of central Africa. Onyalai exhibits similarities to idiopathic thrombocytopenic purpura but differs in pathogenesis. The affected age range is from less than a year to 70 years and seems to not be...
Alloimmune disorders
- Fetomaternal alloimmune thrombocytopenia
- Some transfusion reactions
Disorders leading to platelet dysfunction or reduced count:
- HELLP syndromeHELLP syndromeHELLP syndrome is a life-threatening obstetric complication usually considered to be a variant of pre-eclampsia. Both conditions usually occur during the later stages of pregnancy, or sometimes after childbirth.HELLP is an abbreviation of the main findings:...
- Hemolytic-uremic syndromeHemolytic-uremic syndromeHemolytic-uremic syndrome , abbreviated HUS, is a disease characterized by hemolytic anemia, acute renal failure and a low platelet count . It predominantly, but not exclusively, affects children. Most cases are preceded by an episode of diarrhea caused by E. coli O157:H7, which is acquired as a...
- ChemotherapyChemotherapyChemotherapy is the treatment of cancer with an antineoplastic drug or with a combination of such drugs into a standardized treatment regimen....
- Dengue
Disorders featuring an elevated count:
- ThrombocytosisThrombocytosisThrombocytosis is the presence of high platelet counts in the blood, and can be either primary or reactive...
, including essential thrombocytosisEssential thrombocytosisEssential thrombocythemia is a rare chronic blood disorder characterized by the overproduction of platelets by megakaryocytes in the bone marrow in the absence of an alternative cause. In some cases this disorder may be progressive, and rarely may evolve into acute myeloid leukemia or myelofibrosis...
(elevated counts, either reactive or as an expression of myeloproliferative diseaseMyeloproliferative diseaseThe myeloproliferative diseases are a group of diseases of the bone marrow in which excess cells are produced. They are related to, and may evolve into, myelodysplastic syndrome and acute myeloid leukemia, although the myeloproliferative diseases on the whole have a much better prognosis than...
); may feature dysfunctional platelets
Disorders of platelet adhesion or aggregation:
- Bernard-Soulier syndromeBernard-Soulier syndromeBernard–Soulier syndrome , also called hemorrhagiparous thrombocytic dystrophy, is a rare autosomal recessive coagulopathy that causes a deficiency of glycoprotein Ib , the receptor for von Willebrand factor, which is important in clot formation.The incidence is estimated to be less than 1 in 1...
- Glanzmann's thrombastheniaGlanzmann's thrombastheniaGlanzmann's thrombasthenia is an abnormality of platelets. It is an extremely rare coagulopathy , in which the platelets lack glycoprotein IIb/IIIa...
- Scott's syndromeScott's syndromeScott syndrome is a rare congenital bleeding disorder that is due to a defect in a platelet mechanism required for blood coagulation. When normal platelets are activated, as may occur at sites of vascular injury, phosphatidylserine in the inner leaflet of the platelet membrane is transported to...
- von Willebrand diseaseVon Willebrand diseasevon Willebrand disease is the most common hereditary coagulation abnormality described in humans, although it can also be acquired as a result of other medical conditions. It arises from a qualitative or quantitative deficiency of von Willebrand factor , a multimeric protein that is required for...
- Hermansky-Pudlak SyndromeHermansky-Pudlak syndromeHermansky–Pudlak syndrome is a rare autosomal recessive disorder which results in oculocutaneous albinism , bleeding problems due to a platelet abnormality , and storage of an abnormal fat-protein compound .There are eight classic forms of the disorder, based on the genetic mutation...
- Gray platelet syndromeGray platelet syndromeGray platelet syndrome , or platelet alpha-granule deficiency, is a rare congenital bleeding disorder caused by a reduction or absence of alpha-granules in blood platelets, and the release of proteins normally contained in these granules into the marrow, causing myelofibrosis.GPS is primarily...
Disorders of platelet metabolism
- Decreased cyclooxygenaseCyclooxygenaseCyclooxygenase is an enzyme that is responsible for formation of important biological mediators called prostanoids, including prostaglandins, prostacyclin and thromboxane. Pharmacological inhibition of COX can provide relief from the symptoms of inflammation and pain...
activity, induced or congenital - Storage pool defects, acquired or congenital
Disorders that indirectly compromise platelet function:
- HaemophiliaHaemophiliaHaemophilia is a group of hereditary genetic disorders that impair the body's ability to control blood clotting or coagulation, which is used to stop bleeding when a blood vessel is broken. Haemophilia A is the most common form of the disorder, present in about 1 in 5,000–10,000 male births...
- Wiskott–Aldrich syndrome
Disorders in which platelets play a key role:
- AtherosclerosisAtherosclerosisAtherosclerosis is a condition in which an artery wall thickens as a result of the accumulation of fatty materials such as cholesterol...
- Coronary artery disease, CAD and myocardial infarctionMyocardial infarctionMyocardial infarction or acute myocardial infarction , commonly known as a heart attack, results from the interruption of blood supply to a part of the heart, causing heart cells to die...
, MI - Cerebrovascular diseaseCerebrovascular diseaseCerebrovascular disease is a group of brain dysfunctions related to disease of the blood vessels supplying the brain. Hypertension is the most important cause; it damages the blood vessel lining, endothelium, exposing the underlying collagen where platelets aggregate to initiate a repairing process...
and StrokeStrokeA stroke, previously known medically as a cerebrovascular accident , is the rapidly developing loss of brain function due to disturbance in the blood supply to the brain. This can be due to ischemia caused by blockage , or a hemorrhage...
, CVA (cerebrovascular accident) - Peripheral artery occlusive diseasePeripheral artery occlusive diseasePeripheral vascular disease , commonly referred to as peripheral arterial disease or peripheral artery occlusive disease , refers to the obstruction of large arteries not within the coronary, aortic arch vasculature, or brain. PVD can result from atherosclerosis, inflammatory processes leading to...
(PAOD) - CancerCancerCancer , known medically as a malignant neoplasm, is a large group of different diseases, all involving unregulated cell growth. In cancer, cells divide and grow uncontrollably, forming malignant tumors, and invade nearby parts of the body. The cancer may also spread to more distant parts of the...
- MalariaMalariaMalaria is a mosquito-borne infectious disease of humans and other animals caused by eukaryotic protists of the genus Plasmodium. The disease results from the multiplication of Plasmodium parasites within red blood cells, causing symptoms that typically include fever and headache, in severe cases...
Discovery
Brewer traced the history of the discovery of the platelet. Although red blood cells had been known since van LeeuwenhoekAnton van Leeuwenhoek
Antonie Philips van Leeuwenhoek was a Dutch tradesman and scientist from Delft, Netherlands. He is commonly known as "the Father of Microbiology", and considered to be the first microbiologist...
(1632–1723), it was the German anatomist Max Schultze (1825–1874) who first offered a description of the platelet in his newly founded journal Archiv für mikroscopische Anatomie. He describes "spherules" to be much smaller than red blood cells that are occasionally clumped and may participate in collections of fibrous material
Fibrin
Fibrin is a fibrous, non-globular protein involved in the clotting of blood. It is a fibrillar protein that is polymerised to form a "mesh" that forms a hemostatic plug or clot over a wound site....
. He recommends further study of the findings.
Giulio Bizzozero
Giulio Bizzozero
Giulio Bizzozero was an Italian doctor and medical researcher. He is known as the original discoverer of Helicobacter pylori, the bacteria which is responsible for peptic ulcer disease...
(1846–1901), building on Schultze's findings, used "living circulation" to study blood cells of amphibians microscopically in vivo
In vivo
In vivo is experimentation using a whole, living organism as opposed to a partial or dead organism, or an in vitro controlled environment. Animal testing and clinical trials are two forms of in vivo research...
. He is especially noted for discovering that platelets clump at the site of blood vessel injury, a process that precedes the formation of a blood clot
Thrombus
A thrombus , or blood clot, is the final product of the blood coagulation step in hemostasis. It is achieved via the aggregation of platelets that form a platelet plug, and the activation of the humoral coagulation system...
. This observation confirmed the role of platelets in coagulation
Coagulation
Coagulation is a complex process by which blood forms clots. It is an important part of hemostasis, the cessation of blood loss from a damaged vessel, wherein a damaged blood vessel wall is covered by a platelet and fibrin-containing clot to stop bleeding and begin repair of the damaged vessel...
.
In transfusion medicine

Whole blood
Whole blood is a term used in transfusion medicine for human blood from a standard blood donation. The blood is typically combined with an anticoagulant during the collection process, but is generally otherwise unprocessed...
and pooled to make a therapeutic dose or collected by apheresis
Apheresis
Apheresis is a medical technology in which the blood of a donor or patient is passed through an apparatus that separates out one particular constituent and returns the remainder to the circulation...
, sometimes concurrently with plasma
Blood plasma
Blood plasma is the straw-colored liquid component of blood in which the blood cells in whole blood are normally suspended. It makes up about 55% of the total blood volume. It is the intravascular fluid part of extracellular fluid...
or red blood cells. The industry standard is for platelets to be tested for bacteria
Bacteria
Bacteria are a large domain of prokaryotic microorganisms. Typically a few micrometres in length, bacteria have a wide range of shapes, ranging from spheres to rods and spirals...
before transfusion to avoid septic reactions, which can be fatal. Recently the AABB Industry Standards for Blood Banks and Transfusion Services (5.1.5.1) has allowed for use of pathogen reduction technology as an alternative to bacterial screenings in platelets.
Pooled whole-blood platelets, sometimes called "random" platelets, are made primarily by two methods. In the US, a unit of whole blood is placed into a large centrifuge
Centrifuge
A centrifuge is a piece of equipment, generally driven by an electric motor , that puts an object in rotation around a fixed axis, applying a force perpendicular to the axis...
in what is referred to as a "soft spin." At these settings, the platelets remain suspended in the plasma. The platelet-rich plasma (PRP) is removed from the RBCs, then centrifuged at a faster setting to harvest the platelets from the plasma. In other regions of the world, the unit of whole blood is centrifuged using settings that cause the platelets to become suspended in the "buffy coat" layer, which includes the platelets and the white blood cells. The "buffy coat" is isolated in a sterile bag, suspended in a small amount of red blood cells and plasma, then centrifuged again to separate the platelets and plasma from the red and white blood cells. Regardless of the initial method of preparation, multiple platelets may be combined into one container using a sterile connection device to manufacture a single product with the desired therapeutic dose.
Apheresis platelets are collected using a mechanical device that draws blood from the donor and centrifuges the collected blood to separate out the platelets and other components to be collected. The remaining blood is returned to the donor. The advantage to this method is that a single donation provides at least one therapeutic dose, as opposed to the multiple donations for whole-blood platelets. This means that a recipient is not exposed to as many different donors and has less risk of transfusion-transmitted disease and other complications. Sometimes a person such as a cancer
Cancer
Cancer , known medically as a malignant neoplasm, is a large group of different diseases, all involving unregulated cell growth. In cancer, cells divide and grow uncontrollably, forming malignant tumors, and invade nearby parts of the body. The cancer may also spread to more distant parts of the...
patient that requires routine transfusions of platelets will receive repeated donations from a specific donor to further minimize the risk. Pathogen reduction of platelets using for example, riboflavin and UV light treatments
Pathogen reduction using riboflavin and UV light
Pathogen reduction using riboflavin and UV light is a method by which infectious pathogens in blood for transfusion are inactivated by adding riboflavin and irradiating with UV light. This method reduces the infectious levels of disease-causing agents that may be found in donated blood components,...
can also be carried out to reduce the infectious load of pathogens contained in donated blood products, thereby reducing the risk of transmission of transfusion transmitted diseases.
Platelets are not cross-matched unless they contain a significant amount of red blood cell
Red blood cell
Red blood cells are the most common type of blood cell and the vertebrate organism's principal means of delivering oxygen to the body tissues via the blood flow through the circulatory system...
s (RBCs), which results in a reddish-orange color to the product. This is usually associated with whole-blood platelets, as apheresis methods are more efficient than "soft spin" centrifugation at isolating the specific components of blood. An effort is usually made to issue type specific platelets, but this is not as critical as it is with RBCs.
Platelets collected by either method have a very short shelf life, typically five days. This results in frequent problems with short supply, as testing the donations often requires up to a full day. Since there are no effective preservative solutions for platelets, they lose potency quickly and are best when fresh.
Platelets are stored under constant agitation at 20–24 °C. Storage at room temperature provides an environment where any bacteria that are introduced to the blood component during the collection process may proliferate and subsequently cause bacteremia in the patient. Regulations are in place in the United States that require products to be tested for the presence of bacterial contamination before transfusion.
Platelets, either apheresis or random-donor platelets, can be processed through a volume reduction process. In this process, the platelets are spun in a centrifuge and the excess plasma is removed, leaving 10 to 100 mL of platelet concentrate. Volume-reduced platelets are normally transfused only to neonatal and pediatric patients when a large volume of plasma could overload the child's small circulatory system. The lower volume of plasma also reduces the chances of an adverse transfusion reaction to plasma proteins. Volume reduced platelets have a shelf life of only four hours.

