
Diabetes management
Encyclopedia
Diabetes is a chronic disease with no proven cures but a lot of research is underway. It is associated with an impaired glucose cycle
that alters the patient's metabolism
. Management of this disease may include carefully managing diet, exercising, taking oral diabetes medication, using some form of insulin, and maintaining proper circulation in the extremities. The disease may be further complicated by other external factors such as stress, illness, menses, injection site scarring, and other physiological factors unique to individual patients.
and lipid
s, to minimize the risk of long-term consequences associated with diabetes. They are suggested in clinical practice guidelines released by various national and international diabetes agencies.
The targets are:
In older patients, clinical practice guidelines by the American Geriatrics Society
states "for frail older adults, persons with life expectancy of less than 5 years, and others in whom the risks of intensive glycemic control appear to outweigh the benefits, a less stringent target such as HbA1c of 8% is appropriate".
As diabetes is a prime risk factor for cardiovascular disease
, controlling other risk factors which may give rise to secondary conditions, as well as the diabetes itself, is one of the facets of diabetes management. Checking cholesterol
, LDL, HDL and triglyceride
levels may indicate hyperlipoproteinemia, which may warrant treatment with hypolipidemic drugs. Checking the blood pressure
and keeping it within strict limits (using diet and antihypertensive
treatment) protects against the retinal, renal and cardiovascular complications of diabetes. Regular follow-up by a podiatrist
or other foot health specialists is encouraged to prevent the development of diabetic foot
. Annual eye exams are suggested to monitor for progression of diabetic retinopathy.
The expense, inconvenience and discomfort of frequent blood glucose measurements has been a significant challenge until recently. Recently newer devices which monitor glucose levels on an ongoing basis have been developed, as detailed below.
studied diabetes in 1909-12, then published a large volume, Studies Concerning Glycosuria and Diabetes, (Boston, 1913). He invented a fasting
treatment for diabetes called the Allen treatment for diabetes. His diet was an early attempt at managing diabetes.
Diet management allows control and awareness of the types of nutrients entering the digestive system, and hence allows indirectly, significant control over changes in blood glucose levels. Blood glucose monitoring allows verification of these, and closer control, especially important since some symptoms of diabetes are not easy for the patient to notice without actual measurement.
Other approaches include exercise and other lifestyle changes which impact the glucose cycle.
In addition, a strong partnership between the patient and the primary healthcare provider – general practitioner
or internist – is an essential tool in the successful management of diabetes. Often the primary care doctor makes the initial diagnosis of diabetes and provides the basic tools to get the patient started on a management program. Regular appointments with the primary care physician and a certified diabetes educator
are some of the best things a patient can do in the early weeks after a diagnosis of diabetes. Upon the diagnosis of diabetes, the primary care physician, specialist, or endocrinologist will conduct a full physical and medical examination. A thorough assessment covers topics such as:
Diabetes can be very complicated, and the physician needs to have as much information as possible to help the patient establish an effective management plan. Physicians may often experience data overload resulting from hundreds of blood-glucose readings, insulin dosages and other health factors occurring between regular office visits which must be deciphered during a relatively brief visit with the patient to determine patterns and establish or modify a treatment plan.
The physician can also make referrals to a wide variety of professionals for additional health care support. In the UK a patient training course is available for newly diagnosed diabetics (see DESMOND
).In a large city there may be a diabetes center where several specialists, such as diabetes educators and dietitians, work together as a team. In smaller towns, the health care team may come together a little differently depending on the types of practitioners in the area. By working together, doctors and patients can optimize the healthcare team to successfully manage diabetes over the long term.
, with the result either in mg/dL (milligrams per deciliter in the USA) or mmol/L (millimoles per litre in Canada and Europe) of blood. The average normal person should have a glucose level of around 4.5 to 7.0 mmol/L (80 to 125 mg/dL).
Optimal management of diabetes involves patients measuring and recording their own blood glucose levels. By keeping a diary of their own blood glucose measurements and noting the effect of food and exercise, patients can modify their lifestyle to better control their diabetes. For patients on insulin, patient involvement is important in achieving effective dosing and timing.
Some edible mushrooms are noted for the ability to lower blood sugar levels including Reishi, Maitake Agaricus blazei
as well as some others.
Levels greater than 13-15 mmol/L (230–270 mg/dL) are considered high, and should be monitored closely to ensure that they reduce rather than continue to remain high. The patient is advised to seek urgent medical attention as soon as possible if blood sugar levels continue to rise after 2-3 tests. High blood sugar levels are known as hyperglycemia, which is not as easy to detect as hypoglycemia and usually happens over a period of days rather than hours or minutes. If left untreated, this can result in diabetic coma
and death.
 Prolonged and elevated levels of glucose in the blood, which is left unchecked and untreated, will, over time, result in serious diabetic complications in those susceptible and sometimes even death. There is currently no way of testing for susceptibility to complications. Diabetics are therefore recommended to check their blood sugar levels either daily or every few days. There is also diabetes management software
Prolonged and elevated levels of glucose in the blood, which is left unchecked and untreated, will, over time, result in serious diabetic complications in those susceptible and sometimes even death. There is currently no way of testing for susceptibility to complications. Diabetics are therefore recommended to check their blood sugar levels either daily or every few days. There is also diabetes management software
available from blood testing manufacturers which can display results and trends over time. Type 1 diabetics normally check more often, due to insulin therapy.
A history of blood sugar level results is especially useful for the diabetic to present to their doctor or physician in the monitoring and control of the disease. Failure to maintain a strict regimen of testing can accelerate symptoms of the condition, and it is therefore imperative that any diabetic patient strictly monitor their glucose levels regularly.
) in a person with diabetes mellitus
. Much evidence suggests that many of the long-term complications of diabetes, especially the microvascular complications, result from many years of hyperglycemia
(elevated levels of glucose in the blood). Good glycemic control, in the sense of a "target" for treatment, has become an important goal of diabetes care, although recent research suggests that the complications of diabetes may be caused by genetic factors or, in type 1 diabetics, by the continuing effects of the autoimmune disease which first caused the pancreas to lose its insulin-producing ability.
Because blood sugar levels fluctuate throughout the day and glucose records are imperfect indicators of these changes, the percentage of hemoglobin
which is glycosylated
is used as a proxy measure of long-term glycemic control in research trials and clinical care of people with diabetes. This test, the hemoglobin A1c or glycosylated hemoglobin
reflects average glucoses over the preceding 2–3 months. In nondiabetic persons with normal glucose metabolism the glycosylated hemoglobin is usually 4-6% by the most common methods (normal ranges may vary by method).
"Perfect glycemic control" would mean that glucose levels were always normal (70–130 mg/dl, or 3.9-7.2 mmol/L) and indistinguishable from a person without diabetes. In reality, because of the imperfections of treatment measures, even "good glycemic control" describes blood glucose levels that average somewhat higher than normal much of the time. In addition, one survey of type 2 diabetics found that they rated the harm to their quality of life from intensive interventions to control their blood sugar to be just as severe as the harm resulting from intermediate levels of diabetic complications.
Accepted "target levels" of glucose and glycosylated hemoglobin that are considered good control have been lowered over the last 25 years, because of improvements in the tools of diabetes care, because of increasing evidence of the value of glycemic control in avoiding complications, and by the expectations of both patients and physicians. What is considered "good control" also varies by age and susceptibility of the patient to hypoglycemia
.
In the 1990s the American Diabetes Association
conducted a publicity campaign to persuade patients and physicians to strive for average glucose and hemoglobin A1c values below 200 mg/dl (11 mmol/l) and 8%. Currently many patients and physicians attempt to do better than that.
Poor glycemic control refers to persistently elevated blood glucose and glycosylated hemoglobin levels, which may range from 200–500 mg/dl (11-28 mmol/L) and 9-15% or higher over months and years before severe complications occur.
s to regularly measure their glucose
levels. Glucose monitoring is both expensive (largely due to the cost of the consumable test strips) and requires significant commitment on the part of the patient. The effort and expense may be worthwhile for patients when they use the values to sensibly adjust food, exercise, and oral medications or insulin. These adjustments are generally made by the patients themselves following training by a clinician.
Regular blood testing, especially in type 1 diabetics, is helpful to keep adequate control of glucose levels and to reduce the chance of long term side effect
s of the disease. There are many (at least 20+) different types of blood monitoring devices available on the market today; not every meter suits all patients and it is a specific matter of choice for the patient, in consultation with a physician or other experienced professional, to find a meter that they personally find comfortable to use. The principle of the devices is virtually the same: a small blood sample is collected and measured. In one type of meter, the electrochemical, a small blood sample is produced by the patient using a lancet (a sterile pointed needle). The blood droplet is usually collected at the bottom of a test strip, while the other end is inserted in the glucose meter. This test strip contains various chemicals so that when the blood is applied, a small electrical charge is created between two contacts. This charge will vary depending on the glucose levels within the blood. In older glucose meters, the drop of blood is placed on top of a strip. A chemical reaction occurs and the strip changes color. The meter then measures the color of the strip optically.
Self-testing is clearly important in type I diabetes where the use of insulin therapy risks episodes of hypoglycaemia and home-testing allows for adjustment of dosage on each administration. However its benefit in type 2 diabetes is more controversial as there is much more variation in severity of type 2 cases. It has been suggested that some type 2 patients might do as well with home urine-testing alone. The best use of home blood-sugar monitoring is being researched.
Benefits of control and reduced hospital admission have been reported. However, patients on oral medication who do not self-adjust their drug dosage will miss many of the benefits of self-testing, and so it is questionable in this group. This is particularly so for patients taking monotherapy with metformin who are not at risk of hypoglycaemia. Regular 6 monthly laboratory testing of HbA1c (glycated haemoglobin) provides some assurance of long-term effective control and allows the adjustment of the patient's routine medication dosages in such cases. High frequency of self-testing in type 2 diabetes has not been shown to be associated with improved control. The argument is made, though, that type 2 patients with poor long term control despite home blood glucose monitoring, either have not had this integrated into their overall management, or are long overdue for tighter control by a switch from oral medication to injected insulin.
in relation to the total hemoglobin. Persistent raised plasma glucose levels cause the proportion of these molecules to go up. This is a test that measures the average amount of diabetic control over a period originally thought to be about 3 months (the average red blood cell lifetime), but more recently thought to be more strongly weighted to the most recent 2 to 4 weeks. In the non-diabetic, the HbA1c level ranges from 4.0-6.0%; patients with diabetes mellitus who manage to keep their HbA1c level below 6.5% are considered to have good glycemic control. The HbA1c test is not appropriate if there has been changes to diet or treatment within shorter time periods than 6 weeks or there is disturbance of red cell aging (e.g. recent bleeding or hemolytic anemia
) or a hemoglobinopathy
(e.g. sickle cell disease). In such cases the alternative Fructosamine
test is used to indicate average control in the preceding 2 to 3 weeks.
A study conducted in 2008 used data from the 2002-2004 National Ambulatory Medical Care Survey has used in order to investigate the relationship between counseling/referral for nutrition or exercise and patient factors, provider factors, and geographic location. Overall, counseling/referral for nutrition occurred in 36% of patient visits and counseling/referral for exercise occurred in 18% of patient visits. After adjusting for patient, physician, and practice characteristics, there was no statistically significant association between race and counseling/referral for nutrition.
The American Diabetes Association
in 1994 recommended that 60-70% of caloric intake should be in the form of carbohydrate
s. This is somewhat controversial, with some researchers claiming that 40% is better, while others claim benefits for a high-fiber, 75% carbohydrate diet.
An article summarizing the view of the American Diabetes Association
gives many recommendations and references to the research. One of the conclusions is that caloric intake must be limited to that which is necessary for maintaining a healthy weight. The methodology of the dietary therapy has attracted lots of attentions from many scientific researchers and the protocols are ranging from nutritional balancing to ambulatory diet-care.
or hypoglycemia
. Adequate control of diabetes leads to lower risk of complications associated with unmonitored diabetes including kidney failure (requiring dialysis
or transplant), blindness, heart disease
and limb amputation
. The most prevalent form of medication is hypoglycemic treatment through either oral hypoglycemics and/or insulin
therapy. There is emerging evidence that full-blown diabetes mellitus type 2 can be evaded in those with only mildly impaired glucose tolerance.
Patients with type 1 diabetes mellitus require direct injection of insulin as their bodies cannot produce enough (or even any) insulin. As of 2010, there is no other clinically available form of insulin administration other than injection for patients with type 1: injection can be done by insulin pump
, by jet injector
, or any of several forms of hypodermic needle
. Non-injective methods of insulin administration have been unattainable as the insulin protein breaks down in the digestive tract. There are several insulin application mechanisms under experimental development as of 2004, including a capsule that passes to the liver and delivers insulin into the bloodstream. There have also been proposed vaccines for type I using glutamic acid decarboxylase (GAD), but these are currently not being tested by the pharmaceutical companies that have sublicensed the patents to them.
For type 2 diabetics, diabetic management consists of a combination of diet
, exercise, and weight loss
, in any achievable combination depending on the patient. Obesity is very common in type 2 diabetes and contributes greatly to insulin resistance. Weight reduction and exercise improve tissue sensitivity to insulin and allow its proper use by target tissues. Patients who have poor diabetic control after lifestyle modifications are typically placed on oral hypoglycemics. Some Type 2 diabetics eventually fail to respond to these and must proceed to insulin therapy. A study conducted in 2008 found that increasingly complex and costly diabetes treatments are being applied to an increasing population with type 2 diabetes. Data from 1994 to 2007 was analyzed and it was found that the mean number of diabetes medications per treated patient increased from 1.14 in 1994 to 1.63 in 2007.
Patient education and compliance with treatment is very important in managing the disease. Improper use of medications and insulin can be very dangerous causing hypo- or hyper-glycemic episodes.
requires close monitoring and a great deal of patient education, as improper administration is quite dangerous. For example, when food intake is reduced, less insulin is required. A previously satisfactory dosing may be too much if less food is consumed causing a hypoglycemic
reaction if not intelligently adjusted. Exercise decreases insulin requirements as exercise increases glucose uptake by body cells whose glucose uptake is controlled by insulin, and vice versa. In addition, there are several types of insulin with varying times of onset and duration of action.
Insulin therapy creates risk because of the inability to continuously know a person's blood glucose level and adjust insulin infusion appropriately. New advances in technology have overcome much of this problem. Small, portable insulin infusion pumps are available from several manufacturers. They allow a continuous infusion of small amounts of insulin to be delivered through the skin around the clock, plus the ability to give bolus doses when a person eats or has elevated blood glucose levels. This is very similar to how the pancreas works, but these pumps lack a continuous "feed-back" mechanism. Thus, the user is still at risk of giving too much or too little insulin unless blood glucose measurements are made.
A further danger of insulin treatment is that while diabetic microangiopathy is usually explained as the result of hyperglycemia, studies in rats indicate that the higher than normal level of insulin diabetics inject to control their hyperglycemia may itself promote small blood vessel disease. While there is no clear evidence that controlling hyperglycemia reduces diabetic macrovascular and cardiovascular disease, there are indications that intensive efforts to normalize blood glucose levels may worsen cardiovascular and cause diabetic mortality.
(loss of peripheral vision or visual acuity), or peripheral neuropathy
(loss of feeling in the feet) can impair a driver’s ability to read street signs, control the speed of the vehicle, apply appropriate pressure to the brakes, etc.
Second, hypoglycemia can affect a person’s thinking process, coordination, and state of consciousness. This disruption in brain functioning is called neuroglycopenia. Studies have demonstrated that the effects of neuroglycopenia
impair driving ability. A study involving people with type 1 diabetes found that individuals reporting two or more hypoglycemia-related driving mishaps differ physiologically and behaviorally from their counterparts who report no such mishaps. For example, during hypoglycemia, drivers who had two or more mishaps reported fewer warning symptoms, their driving was more impaired, and their body released less epinephrine (a hormone that helps raise BG). Additionally, individuals with a history of hypoglycemia-related driving mishaps appear to use sugar at a faster rate and are relatively slower at processing information. These findings indicate that although anyone with type 1 diabetes may be at some risk of experiencing disruptive hypoglycemia while driving, there is a subgroup of type 1 drivers who are more vulnerable to such events.
Given the above research findings, it is recommended that drivers with type 1 diabetes with a history of driving mishaps should never drive when their BG is less than 70 mg/dl. Instead, these drivers are advised to treat hypoglycemia and delay driving until their BG is above 90 mg/dl. Such drivers should also learn as much as possible about what causes their hypoglycemia, and use this information to avoid future hypoglycemia while driving.
Studies funded by the National Institutes of Health (NIH) have demonstrated that face-to-face training programs designed to help individuals with type 1 diabetes better anticipate, detect, and prevent extreme BG can reduce the occurrence of future hypoglycemia-related driving mishaps. An internet-version of this training has also been shown to have significant beneficial results. Additional NIH funded research to develop internet interventions specifically to help improve driving safety in drivers with type 1 diabetes is currently underway.
, based on the saliva
of a Gila monster
, to control blood sugar in patients with type 2 diabetes.
researcher Dr. Cynthia Marling, of the Ohio University
Russ College of Engineering and Technology, in collaboration with the Appalachian Rural Health Institute Diabetes Center, is developing a case based reasoning system to aid in diabetes management. The goal of the project is to provide automated intelligent decision support to diabetes patients and their professional care providers by interpreting the ever increasing quantities of data provided by current diabetes management technology and translating it into better care without time consuming manual effort on the part of an endocrinologist or diabetologist. This type of Artificial Intelligence
-based treatment shows some promise with initial testing of a prototype
system producing best practice
treatment advice which anaylizing physicians deemed to have some degree of benefit over 70% of the time and advice of neutral benefit another nearly 25% of the time.
Use of a "Diabetes Coach" is becoming an increasingly popular way to manage diabetes. A Diabetes Coach is usually a Certified diabetes educator
(CDE) who is trained to help people in all aspects of caring for their diabetes. The CDE can advise the patient on diet, medications, proper use of insulin injections and pumps, exercise, and other ways to manage diabetes while living a healthy and active lifestyle. CDEs can be found locally or by contacting a company which provides personalized diabetes care using CDEs. Diabetes Coaches can speak to a patient on a pay-per-call basis or via a monthly plan.
and teeth problems, especially in after puberty
and aging individuals. Diabetic patients have greater chances of developing oral health problems such as tooth decay, salivary gland
dysfunction, fungal infections, inflammatory skin
disease, periodontal disease
or taste impairment and thrush of the mouth. The oral problems in persons suffering from diabetes can be prevented with a good control of the blood sugar levels, regular checkups and a very good oral hygiene
. By maintaining a good oral status, diabetic persons prevent losing their teeth as a result of various periodontal conditions.
Diabetic persons must increase their awareness towards the oral infections as they have a double impact on one's health. Firstly, people with diabetes are more likely to develop periodontal disease which causes increased blood sugar levels, often leading to diabetes complications. Severe periodontal disease can increase blood sugar, contributing to increased periods of time when the body functions with a high blood sugar. This puts diabetics at increased risk for diabetic complications.
The first symptoms of gum and teeth infections in diabetic persons are decreased salivary flow, burning mouth or tongue
. Also, patients may experience signs as dry mouth which increases the incidence of decay. Poorly-controlled diabetes usually leads to gum problems recession as plaque
creates more harmful proteins in the gums.
Tooth decay and cavities are some of the first oral problems that individuals with diabetes are at risk for. Increased blood sugar levels translate into greater sugars and acids that attack the teeth and lead to gum diseases. Gingivitis
can also occur as a result of increased blood sugar levels along with an inappropriate oral hygiene. Periodontitis is an oral disease caused by untreated gingivitis and which destroys the soft tissue and bone that support the teeth. This disease may cause the gums to pull away from the teeth which may eventually loosen and fall out. Diabetic people tend to experience more severe periodontitis because diabetes lowers the ability to resist infection and also slows healing. At the same time, an oral infection such as periodontitis can make diabetes more difficult to control because it causes the blood sugar levels to rise.
To prevent further diabetic complications as well as serious oral problems, diabetic persons must keep their blood sugar levels under control and have a proper oral hygiene. A study in the Journal of Periodontology found that poorly controlled type 2 diabetic patients are more likely to develop periodontal disease than well-controlled diabetics are. At the same time, diabetic patients are recommended to have regular checkups with a dental care provider at least once in three to four months. Diabetics who receive good dental care and have good insulin control typically have a better chance at avoiding gum disease to help prevent tooth loss
.
Dental care is therefore even more important for diabetic patients than for healthy individuals. Maintaining the teeth and gum healthy is done by taking some preventing measures such as regular appointments at a dentist and a very good oral hygiene. Also, oral health problems can be avoided by closely monitoring the blood sugar levels. Patients who keep better under control their blood sugar levels and diabetes are less likely to develop oral health problems when compared to diabetic patients who control their disease moderately or poorly.
Poor oral hygiene is a great factor to take under consideration when it comes to oral problems and even more in people with diabetes. Diabetic people are advised to brush their teeth at least twice a day, and if possible, after all meals and snacks. However, brushing in the morning and at night is mandatory as well as flossing and using an anti-bacterial mouthwash
. Individuals who suffer from diabetes are recommended to use toothpaste
that contains fluoride
as this has proved to be the most efficient in fighting oral infections and tooth decay. Flossing must be done at least once a day, as well because it is helpful in preventing oral problems by removing the plaque between the teeth, which is not removed when brushing.
Diabetic patients must get professional dental cleanings every six months. In cases when dental surgery
is needed, it is necessary to take some special precautions such as adjusting diabetes medication or taking antibiotics to prevent infection. Looking for early signs of gum disease (redness, swelling, bleeding gums
) and informing the dentist about them is also helpful in preventing further complications. Quitting smoking is recommended to avoid serious diabetes complications and oral diseases.
Diabetic persons are advised to make morning appointments to the dental care provider as during this time of the day the blood sugar levels tend to be better kept under control. Not least, individuals who suffer from diabetes must make sure both their physician and dental care provider are informed and aware of their condition, medical history and periodontal status.
for diabetes mellitus type 1. However, in October 2010, Mayo Clinic and the University of Minnesota launched a campaign to optimally treat and ultimately cure the disease within a decade.
Diabetes type 1 is caused by the destruction of enough beta cell
s to produce symptoms; these cells, which are found in the Islets of Langerhans
in the pancreas
, produce and secrete insulin
, the single hormone responsible for allowing glucose
to enter from the blood
into cell
s (in addition to the hormone amylin
, another hormone required for glucose homeostasis
). Hence, the phrase "curing diabetes type 1" means "causing a maintenance or restoration of the endogenous
ability of the body to produce insulin in response to the level of blood glucose" and cooperative operation with counterregulatory hormones.
This section deals only with approaches for curing the underlying condition of diabetes type 1, by enabling the body to endogenously, in vivo, produce insulin in response to the level of blood glucose. It does not cover other approaches, such as, for instance, closed-loop integrated glucometer/insulin pump products, which could potentially increase the quality-of-life for some who have diabetes type 1, and may by some be termed "artificial pancreas".
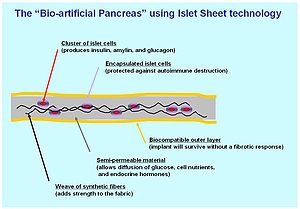 A biological approach to the artificial pancreas is to implant bioengineered tissue
A biological approach to the artificial pancreas is to implant bioengineered tissue
containing islet cells
, which would secrete the amounts of insulin, amylin
and glucagon needed in response to sensed glucose.
When islet cells have been transplanted via the Edmonton protocol
, insulin production (and glycemic control) was restored, but at the expense of continued immunosuppression
drugs. Encapsulation
of the islet cells in a protective coating has been developed to block the immune response to transplanted cells, which relieves the burden of immunosuppression and benefits the longevity of the transplant.
One concept of the bio-artificial pancreas uses encapsulated islet cells to build an islet sheet which can be surgically implanted to function as an artificial pancreas.
This islet sheet design consists of:
Islet sheet with encapsulation research is pressing forward with large animal studies at the present, with plans for human clinical trials within a few years.
Clinical studies underway in New Zealand by Living Cell Technologies have encapsulated pig islet cells in a seaweed derived capsule. This approach has had very positive clinical studies and is currently underway in human trials as of 2008. So far, treatment using this method of cell encapsulation has been proven safe and effective and is the first to achieve insulin independence in human trials without immunosuppressant drugs.
between 2001 and 2003 demonstrated a protocol to reverse type 1 diabetes in non-obese diabetic mice (a frequently used animal model for type 1 diabetes mellitus). Three other institutions have had similar results, as published in the March 24, 2006 issue of Science
. A fourth study by the National Institutes of Health
achieved similar results, and also sheds light on the biological mechanisms involved.
Other researchers, most notably Dr. Aaron I. Vinik of the Strelitz Diabetes Research Institute of Eastern Virginia Medical School and a former colleague, Dr. Lawrence Rosenberg (now at McGill University
) discovered in a protein they refer to as INGAP, which stands for Islet Neogenesis Associated Protein back in 1997. INGAP seems to be the product of a gene responsible for regenerating the islets that make insulin and other important hormones in the pancreas.
INGAP has had commercialization difficulties. Although it has appeared promising, commercial rights have changed hands repeatedly, having once been owned by Procter & Gamble Pharmaceuticals, which eventually dropped it. Rights were then acquired by GMP Companies. More recently, Kinexum Metabolics, Inc. has since sublicensed INGAP from GMP for further clinical trials. Kinexum has continued development under Dr. G. Alexander Fleming, an experienced metabolic drug developer, who headed diabetes drug review at the FDA for over a decade. As of 2008, the protein had undergone Phase 2 Human Clinical Trials, and developers were analyzing the results. At the American Diabetes Association's 68th Annual Scientific Sessions in San Francisco, Kinexum announced a Phase 2 human clinical trial with a combination therapy, consisting of DiaKine's Lisofylline (LSF) and Kinexum's INGAP peptide, which is expected to begin in late 2008. The trial will be unique in that patients who are beyond the 'newly diagnosed' period will be included in the study. Most current trials seeking to treat people with type 1 diabetes do not include those with established disease.
s.
South Korea
In January 2006, a team of South Korean scientists has grown pancreatic beta cells, which can help treat diabetes, from stem cells taken from the umbilical cord blood of newborn babies.
Brazil
Stem cell research has also been suggested as a potential avenue for a cure since it may permit regrowth of Islet cells which are genetically part of the treated individual, thus perhaps eliminating the need for immuno-suppressants.[48] This new method autologous nonmyeloablative hematopoietic stem cell transplantation was developed by a research team composed by Brazilian and American scientists (Dr. Julio Voltarelli, Dr. Carlos Eduardo Couri, Dr Richard Burt, and colleagues) and it was the first study to use stem cell therapy in human diabetes mellitus This was initially tested in mice and in 2007 there was the first publication of stem cell therapy to treat this form of diabetes. Until 2009, there was 23 patients included and followed for a mean period of 29.8 months (ranging from 7 to 58 months). In the trial, severe immunosuppression with high doses of cyclophosphamide and anti-thymocyte globulin is used with the aim of "turning off" the immunologic system", and then autologous hematopoietic stem cells are reinfused to regenerate a new one. In summary it is a kind of "immunologic reset" that blocks the autoimmune attack against residual pancreatic insulin-producing cells. Until December 2009, 12 patients remained continuously insulin-free for periods raging from 14 to 52 months and 8 patients became transiently insulin-free for periods ranging from 6 to 47 months. Of these last 8 patients, 2 became insulin-free again after the use of sitagliptin, a DPP-4 inhibitor approved only to treat type 2 diabetic patients and this is also the first study to document the use and complete insulin-independendce in humans with type 1 diabetes with this medication. In parallel with insulin suspension, indirect measures of endogenous insulin secretion revealed that it significantly increased in the whole group of patients, regardless the need of daily exogenous insulin use.
However, there were no control subjects, which means that all of the processes could have been completely or partially natural. Secondly, no theory for the mechanism of cure has been promoted. It is too early to say whether the results will be positive or negative in the long run.
University of North Carolina
In September 2008, scientists from the University of North Carolina at Chapel Hill School of Medicine have announced their success in transforming cells from human skin into cells that produce insulin.
The skin cells were first transformed into stem cells and then had been differentiated into insulin-secreting cells.
However, other scientists have doubts, as the research papers fail to detail the new cells' glucose responsiveness and the amount of insulin they are capable of producing.
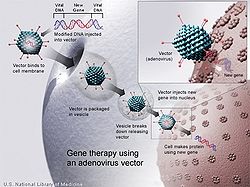 Technology for gene therapy
Technology for gene therapy
is advancing rapidly such that there are multiple pathways possible to support endocrine function, with potential to practically cure diabetes.
Yonsei University
Scientists in the South Korea
n university of Yonsei
have, in 2000, succeeded in reversing diabetes in mice
and rat
s. Using a viral vector, a DNA encoding the production of an insulin analog was injected to the animals, which remained non-diabetic for at least the eight months duration of the study.
There is no practical cure, at this time, for type 1 diabetes. The fact that type 1 diabetes is due to the failure of one of the cell types of a single organ with a relatively simple function (i.e. the failure of the beta cells in the Islets of Langerhans) has led to the study of several possible schemes to cure this form of diabetes mostly by replacing the pancreas or just the beta cells. Only those type 1 diabetics who have received either a pancreas or a kidney-pancreas transplant (often when they have developed diabetic kidney disease (i.e., nephropathy) and become insulin-independent) may now be considered "cured" from their diabetes. A simultaneous pancreas-kidney transplant is a promising solution, showing similar or improved survival rates over a kidney transplant alone. Still, they generally remain on long-term immunosuppressive drug
s and there is a possibility that the immune system will mount a host versus graft response against the transplanted organ.
Transplants of exogenous beta cells have been performed experimentally in both mice and humans, but this measure is not yet practical in regular clinical practice partly due to the limited number of beta cell donors. Thus far, like any such transplant, it has provoked an immune reaction and long-term immunosuppressive drugs have been needed to protect the transplanted tissue. An alternative technique has been proposed to place transplanted beta cells in a semi-permeable container, isolating and protecting them from the immune system. Stem cell research has also been suggested as a potential avenue for a cure since it may permit regrowth of Islet cells which are genetically part of the treated individual, thus perhaps eliminating the need for immuno-suppressants.
This new method autologous nonmyeloablative hematopoietic stem cell transplantation was developed by a research team composed by Brazilian and American scientists (Dr. Julio Voltarelli, Dr. Carlos Eduardo Couri, Dr Richard Burt, and colleagues) and it was the first study to use stem cell therapy in human diabetes mellitus. This was initially tested in mice and in 2007 there was the first publication of stem cell therapy to treat this form of diabetes. Until 2009, there was 23 patients included and followed for a mean period of 29.8 months (ranging from 7 to 58 months). In the trial, severe immunosuppression with high doses of cyclophosphamide and anti-thymocyte globulin is used with the aim of "turning off" the immunologic system", and then autologous hematopoietic stem cells are reinfused to regenerate a new one. In summary it is a kind of "immunologic reset" that blocks the autoimmune attack against residual pancreatic insulin-producing cells. Until December 2009, 12 patients remained continuously insulin-free for periods raging from 14 to 52 months and 8 patients became transiently insulin-free for periods ranging from 6 to 47 months. Of these last 8 patients, 2 became insulin-free again after the use of sitagliptin, a DPP-4 inhibitor approved only to treat type 2 diabetic patients and this is also the first study to document the use and complete insulin-independendce in humans with type 1 diabetes with this medication. In parallel with insulin suspension, indirect measures of endogenous insulin secretion revealed thate it significantly increased in the whole group of patients, regardless the need of daily exogenous insulin use.
Microscopic or nanotechnological approaches are under investigation as well, in one proposed case with implanted stores of insulin metered out by a rapid response valve sensitive to blood glucose levels. At least two approaches have been demonstrated in vitro. These are, in some sense, closed-loop insulin pumps.
and reducing sugar
and carbohydrate
intake with a goal of losing weight
. These can restore insulin sensitivity even when the weight loss is modest, for example around 5 kg (10 to 15 lb), most especially when it is in abdominal fat deposits. Diets that are very low in saturated fats have been claimed to reverse insulin resistance.
Testosterone replacement therapy may improve glucose tolerance and insulin sensitivity in diabetic hypogonadal men. The mechanisms by which testosterone
decreases insulin resistance
is under study. Moreover testosterone may have a protective effect on pancreatic beta cells, which is possibly exerted by androgen-receptor-mediated mechanisms and influence of inflammatory cytokines.
Recently it has been suggested that a type of gastric bypass surgery
may normalize blood glucose levels in 80-100% of severely obese patients with diabetes. The precise causal mechanisms are being intensively researched; its results may not simply be attributable to weight loss, as the improvement in blood sugars seems to precede any change in body mass. This approach may become a treatment for some people with type 2 diabetes, but has not yet been studied in prospective clinical trials. This surgery may have the additional benefit of reducing the death rate from all causes by up to 40% in severely obese people. A small number of normal to moderately obese patients with type 2 diabetes have successfully undergone similar operations.
MODY is another classification of diabetes and it can be treated by early lifesyle management and medical management. it has to be treated in the early stage, so as to provide a good health.
Glucose cycle
The glucose cycle occurs primarily in the liver and is the dynamic equilibrium between glucose and glucose 6-phosphate. This is important for maintaining a constant concentration of glucose in the blood stream....
that alters the patient's metabolism
Metabolism
Metabolism is the set of chemical reactions that happen in the cells of living organisms to sustain life. These processes allow organisms to grow and reproduce, maintain their structures, and respond to their environments. Metabolism is usually divided into two categories...
. Management of this disease may include carefully managing diet, exercising, taking oral diabetes medication, using some form of insulin, and maintaining proper circulation in the extremities. The disease may be further complicated by other external factors such as stress, illness, menses, injection site scarring, and other physiological factors unique to individual patients.
Goals
The treatment goals for type 2 diabetic patients are related to effective control of blood glucose, blood pressureBlood pressure
Blood pressure is the pressure exerted by circulating blood upon the walls of blood vessels, and is one of the principal vital signs. When used without further specification, "blood pressure" usually refers to the arterial pressure of the systemic circulation. During each heartbeat, BP varies...
and lipid
Lipid
Lipids constitute a broad group of naturally occurring molecules that include fats, waxes, sterols, fat-soluble vitamins , monoglycerides, diglycerides, triglycerides, phospholipids, and others...
s, to minimize the risk of long-term consequences associated with diabetes. They are suggested in clinical practice guidelines released by various national and international diabetes agencies.
The targets are:
- HbA1c of 6% to 7.0%
- Preprandial blood glucose: 4.0 to 6.0 mmol/L (72 to 108 mg/dl)
- 2-hour postprandialPostprandialPostprandial means after eating a meal while preprandial is before a meal.-Usages of the term:This term is used in many contexts but also in relation to blood sugar levels, which are normally measured 2 hours after and before eating in a postprandial glucose test...
blood glucose: 5.0 to 8.0 mmol/L (90 to 144 mg/dl)
In older patients, clinical practice guidelines by the American Geriatrics Society
American Geriatrics Society
The American Geriatrics Society : a professional society founded on June 11, 1942 for doctors practicing geriatric medicine. Among the founding physicians were Dr. Ignatz Leo Nascher, who coined the term "geriatrics," Dr. Malford W. Thewlis, who was named the first executive secretary of the...
states "for frail older adults, persons with life expectancy of less than 5 years, and others in whom the risks of intensive glycemic control appear to outweigh the benefits, a less stringent target such as HbA1c of 8% is appropriate".
Issues
The primary issue requiring management is that of the glucose cycle. In this, glucose in the bloodstream is made available to cells in the body; a process dependent upon the twin cycles of glucose entering the bloodstream, and insulin allowing appropriate uptake into the body cells. Both aspects can require management.Complexities
The main complexities stem from the nature of the feedback loop of the glucose cycle, which is sought to be regulated:- The glucose cycle is a system which is affected by two factors: entry of glucose into the bloodstream and also blood levels of insulin to control its transport out of the bloodstream
- As a system, it is sensitive to diet and exercise
- It is affected by the need for user anticipation due to the complicating effects of time delays between any activity and the respective impact on the glucose system
- Management is highly intrusive, and compliance is an issue, since it relies upon user lifestyle change and often upon regular sampling and measuring of blood glucose levels, multiple times a day in many cases
- It changes as people grow and develop
- It is highly individual
As diabetes is a prime risk factor for cardiovascular disease
Cardiovascular disease
Heart disease or cardiovascular disease are the class of diseases that involve the heart or blood vessels . While the term technically refers to any disease that affects the cardiovascular system , it is usually used to refer to those related to atherosclerosis...
, controlling other risk factors which may give rise to secondary conditions, as well as the diabetes itself, is one of the facets of diabetes management. Checking cholesterol
Cholesterol
Cholesterol is a complex isoprenoid. Specifically, it is a waxy steroid of fat that is produced in the liver or intestines. It is used to produce hormones and cell membranes and is transported in the blood plasma of all mammals. It is an essential structural component of mammalian cell membranes...
, LDL, HDL and triglyceride
Triglyceride
A triglyceride is an ester derived from glycerol and three fatty acids. There are many triglycerides, depending on the oil source, some are highly unsaturated, some less so....
levels may indicate hyperlipoproteinemia, which may warrant treatment with hypolipidemic drugs. Checking the blood pressure
Blood pressure
Blood pressure is the pressure exerted by circulating blood upon the walls of blood vessels, and is one of the principal vital signs. When used without further specification, "blood pressure" usually refers to the arterial pressure of the systemic circulation. During each heartbeat, BP varies...
and keeping it within strict limits (using diet and antihypertensive
Antihypertensive
The antihypertensives are a class of drugs that are used to treat hypertension . Evidence suggests that reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34%, of ischaemic heart disease by 21%, and reduce the likelihood of dementia, heart failure, and mortality from...
treatment) protects against the retinal, renal and cardiovascular complications of diabetes. Regular follow-up by a podiatrist
Podiatry
Podiatry is a branch of medicine devoted to the study, diagnosis, and treatment of disorders of the foot, ankle, and lower leg. The term podiatry came into use first in the early 20th century United States, where it now denotes a Doctor of Podiatric Medicine , a specialist who is qualified by their...
or other foot health specialists is encouraged to prevent the development of diabetic foot
Diabetic foot
Diabetic foot ulcer is one of the major complications of diabetes mellitus, and probably the major component of the diabetic foot. It occurs in 15% of all patients with diabetes and precedes 84% of all lower leg amputations...
. Annual eye exams are suggested to monitor for progression of diabetic retinopathy.
The expense, inconvenience and discomfort of frequent blood glucose measurements has been a significant challenge until recently. Recently newer devices which monitor glucose levels on an ongoing basis have been developed, as detailed below.
Early advancements
Late in the nineteenth century, sugar in the urine (glycosuria) was associated with diabetes. Various doctors studied the connection. Frederick Madison AllenFrederick Madison Allen
Frederick Madison Allen was a doctor who is perhaps best remembered today for his work on a diet for sufferers of diabetes mellitus. Born in Iowa, he later studied medicine in California, after which time he was employed in a poorly paid position at Harvard University, before his work in New...
studied diabetes in 1909-12, then published a large volume, Studies Concerning Glycosuria and Diabetes, (Boston, 1913). He invented a fasting
Fasting
Fasting is primarily the act of willingly abstaining from some or all food, drink, or both, for a period of time. An absolute fast is normally defined as abstinence from all food and liquid for a defined period, usually a single day , or several days. Other fasts may be only partially restrictive,...
treatment for diabetes called the Allen treatment for diabetes. His diet was an early attempt at managing diabetes.
Modern approaches
Modern approaches to diabetes primarily rely upon dietary and lifestyle management, often combined with regular ongoing blood glucose level monitoring.Diet management allows control and awareness of the types of nutrients entering the digestive system, and hence allows indirectly, significant control over changes in blood glucose levels. Blood glucose monitoring allows verification of these, and closer control, especially important since some symptoms of diabetes are not easy for the patient to notice without actual measurement.
Other approaches include exercise and other lifestyle changes which impact the glucose cycle.
In addition, a strong partnership between the patient and the primary healthcare provider – general practitioner
General practitioner
A general practitioner is a medical practitioner who treats acute and chronic illnesses and provides preventive care and health education for all ages and both sexes. They have particular skills in treating people with multiple health issues and comorbidities...
or internist – is an essential tool in the successful management of diabetes. Often the primary care doctor makes the initial diagnosis of diabetes and provides the basic tools to get the patient started on a management program. Regular appointments with the primary care physician and a certified diabetes educator
Certified diabetes educator
A certified diabetes educator is a health care professional who is specialized and certified to teach people with diabetes how to manage their condition....
are some of the best things a patient can do in the early weeks after a diagnosis of diabetes. Upon the diagnosis of diabetes, the primary care physician, specialist, or endocrinologist will conduct a full physical and medical examination. A thorough assessment covers topics such as:
- Height and weight measurements
- Blood pressure measurements
- Thyroid examination
- Examination of hands, fingers, feet, and toes for circulatory abnormalities
- Blood tests for fasting blood sugar, A1c, and cholesterol
- Family history of diabetes, cardiovascular disease, and strokeStrokeA stroke, previously known medically as a cerebrovascular accident , is the rapidly developing loss of brain function due to disturbance in the blood supply to the brain. This can be due to ischemia caused by blockage , or a hemorrhage...
- Prior infections and medical conditions
- A list of current medications, including:
- Prescription medications
- Over-the-counter medications
- VitaminVitaminA vitamin is an organic compound required as a nutrient in tiny amounts by an organism. In other words, an organic chemical compound is called a vitamin when it cannot be synthesized in sufficient quantities by an organism, and must be obtained from the diet. Thus, the term is conditional both on...
, mineral or herbal supplements
- Smoking history, including encouragement to stop smoking (if applicable)
- Signs of complications with pregnancy or trying to get pregnant for women patients
- Eating and exercise habits
- Vision abnormalities, to check for eye health issues
- Urination abnormalities, which can indicate kidney disease
Diabetes can be very complicated, and the physician needs to have as much information as possible to help the patient establish an effective management plan. Physicians may often experience data overload resulting from hundreds of blood-glucose readings, insulin dosages and other health factors occurring between regular office visits which must be deciphered during a relatively brief visit with the patient to determine patterns and establish or modify a treatment plan.
The physician can also make referrals to a wide variety of professionals for additional health care support. In the UK a patient training course is available for newly diagnosed diabetics (see DESMOND
DESMOND (diabetes)
DESMOND is a UK NHS training course for people with type 2 diabetes that helps people to identify their own health risks and to set their own goals.- Background :...
).In a large city there may be a diabetes center where several specialists, such as diabetes educators and dietitians, work together as a team. In smaller towns, the health care team may come together a little differently depending on the types of practitioners in the area. By working together, doctors and patients can optimize the healthcare team to successfully manage diabetes over the long term.
Blood sugar level
Blood sugar level is measured by means of a glucose meterGlucose meter
A glucose meter is a medical device for determining the approximate concentration of glucose in the blood. It is a key element of home blood glucose monitoring by people with diabetes mellitus or hypoglycemia...
, with the result either in mg/dL (milligrams per deciliter in the USA) or mmol/L (millimoles per litre in Canada and Europe) of blood. The average normal person should have a glucose level of around 4.5 to 7.0 mmol/L (80 to 125 mg/dL).
Optimal management of diabetes involves patients measuring and recording their own blood glucose levels. By keeping a diary of their own blood glucose measurements and noting the effect of food and exercise, patients can modify their lifestyle to better control their diabetes. For patients on insulin, patient involvement is important in achieving effective dosing and timing.
Some edible mushrooms are noted for the ability to lower blood sugar levels including Reishi, Maitake Agaricus blazei
Agaricus blazei
Agaricus subrufescens is a species of mushroom, commonly known as almond mushroom, mushroom of the sun, God's mushroom, mushroom of life, royal sun agaricus, jisongrong or himematsutake and by a number of other...
as well as some others.
Hypo and hyperglycemia
Levels which are significantly above or below this range are problematic and can in some cases be dangerous. A level of <3.8 mmol/L (<70 mg/dL) is usually described as a hypoglycemic attack (low blood sugar). Most diabetics know when they are going to "go hypo" and usually are able to eat some food or drink something sweet to raise levels. A patient who is hyperglycemic (high glucose) can also become temporarily hypoglycemic, under certain conditions (e.g. not eating regularly, or after strenuous exercise, followed by fatigue). Intensive efforts to achieve blood sugar levels close to normal have been shown to triple the risk of the most severe form of hypoglycemia, in which the patient requires assistance from by-standers in order to treat the episode. There were annually 48,500 hospitalizations for diabetic hypoglycemia and 13,100 for diabetic hypoglycemia resulting in coma in the period 1989 to 1991, before intensive blood sugar control was as widely recommended as today. One study found that hospital admissions for diabetic hypoglycemia increased by 50% from 1990-1993 to 1997-2000, as strict blood sugar control efforts became more common. Among intensively controlled type 1 diabetics, 55% of episodes of severe hypoglycemia occur during sleep, and 6% of all deaths in diabetics under the age of 40 are from nocturnal hypoglycemia in the so-called 'dead-in-bed syndrome,' while National Institute of Health statistics show that 2% to 4% of all deaths in diabetics are from hypoglycemia. In children and adolescents following intensive blood sugar control, 21% of hypoglycemic episodes occurred without explanation. In addition to the deaths caused by diabetic hypoglycemia, periods of severe low blood sugar can also cause permanent brain damage. Interestingly, although diabetic nerve disease is usually associated with hyperglycemia, hypoglycemia as well can initiate or worsen neuropathy in diabetics intensively struggling to reduce their hyperglycemia.Levels greater than 13-15 mmol/L (230–270 mg/dL) are considered high, and should be monitored closely to ensure that they reduce rather than continue to remain high. The patient is advised to seek urgent medical attention as soon as possible if blood sugar levels continue to rise after 2-3 tests. High blood sugar levels are known as hyperglycemia, which is not as easy to detect as hypoglycemia and usually happens over a period of days rather than hours or minutes. If left untreated, this can result in diabetic coma
Diabetic coma
Diabetic coma is a reversible form of coma found in people with diabetes mellitus. It is a medical emergency.Three different types of diabetic coma are identified:#Severe diabetic hypoglycemia...
and death.

Diabetes management software
Diabetes Management Software refers to software tools that run on personal computers and personal digital assistants to help persons with Type 1 and Type 2 diabetes manage the data associated with:*test results from a glucose meter*diabetes logbooks...
available from blood testing manufacturers which can display results and trends over time. Type 1 diabetics normally check more often, due to insulin therapy.
A history of blood sugar level results is especially useful for the diabetic to present to their doctor or physician in the monitoring and control of the disease. Failure to maintain a strict regimen of testing can accelerate symptoms of the condition, and it is therefore imperative that any diabetic patient strictly monitor their glucose levels regularly.
Glycemic control
Glycemic control is a medical term referring to the typical levels of blood sugar (glucoseGlucose
Glucose is a simple sugar and an important carbohydrate in biology. Cells use it as the primary source of energy and a metabolic intermediate...
) in a person with diabetes mellitus
Diabetes mellitus
Diabetes mellitus, often simply referred to as diabetes, is a group of metabolic diseases in which a person has high blood sugar, either because the body does not produce enough insulin, or because cells do not respond to the insulin that is produced...
. Much evidence suggests that many of the long-term complications of diabetes, especially the microvascular complications, result from many years of hyperglycemia
Hyperglycemia
Hyperglycemia or Hyperglycæmia, or high blood sugar, is a condition in which an excessive amount of glucose circulates in the blood plasma. This is generally a glucose level higher than 13.5mmol/l , but symptoms may not start to become noticeable until even higher values such as 15-20 mmol/l...
(elevated levels of glucose in the blood). Good glycemic control, in the sense of a "target" for treatment, has become an important goal of diabetes care, although recent research suggests that the complications of diabetes may be caused by genetic factors or, in type 1 diabetics, by the continuing effects of the autoimmune disease which first caused the pancreas to lose its insulin-producing ability.
Because blood sugar levels fluctuate throughout the day and glucose records are imperfect indicators of these changes, the percentage of hemoglobin
Hemoglobin
Hemoglobin is the iron-containing oxygen-transport metalloprotein in the red blood cells of all vertebrates, with the exception of the fish family Channichthyidae, as well as the tissues of some invertebrates...
which is glycosylated
Glycosylation
Glycosylation is the reaction in which a carbohydrate, i.e. a glycosyl donor, is attached to a hydroxyl or other functional group of another molecule . In biology glycosylation refers to the enzymatic process that attaches glycans to proteins, lipids, or other organic molecules...
is used as a proxy measure of long-term glycemic control in research trials and clinical care of people with diabetes. This test, the hemoglobin A1c or glycosylated hemoglobin
Glycosylated hemoglobin
Glycated hemoglobin is a form of hemoglobin that is measured primarily to identify the average plasma glucose concentration over prolonged periods of time. It is formed in a non-enzymatic glycation pathway by hemoglobin's exposure to plasma glucose...
reflects average glucoses over the preceding 2–3 months. In nondiabetic persons with normal glucose metabolism the glycosylated hemoglobin is usually 4-6% by the most common methods (normal ranges may vary by method).
"Perfect glycemic control" would mean that glucose levels were always normal (70–130 mg/dl, or 3.9-7.2 mmol/L) and indistinguishable from a person without diabetes. In reality, because of the imperfections of treatment measures, even "good glycemic control" describes blood glucose levels that average somewhat higher than normal much of the time. In addition, one survey of type 2 diabetics found that they rated the harm to their quality of life from intensive interventions to control their blood sugar to be just as severe as the harm resulting from intermediate levels of diabetic complications.
Accepted "target levels" of glucose and glycosylated hemoglobin that are considered good control have been lowered over the last 25 years, because of improvements in the tools of diabetes care, because of increasing evidence of the value of glycemic control in avoiding complications, and by the expectations of both patients and physicians. What is considered "good control" also varies by age and susceptibility of the patient to hypoglycemia
Hypoglycemia
Hypoglycemia or hypoglycæmia is the medical term for a state produced by a lower than normal level of blood glucose. The term literally means "under-sweet blood"...
.
In the 1990s the American Diabetes Association
American Diabetes Association
The American Diabetes Association is a United States-based association working to fight the consequences of diabetes, and to help those affected by diabetes...
conducted a publicity campaign to persuade patients and physicians to strive for average glucose and hemoglobin A1c values below 200 mg/dl (11 mmol/l) and 8%. Currently many patients and physicians attempt to do better than that.
Poor glycemic control refers to persistently elevated blood glucose and glycosylated hemoglobin levels, which may range from 200–500 mg/dl (11-28 mmol/L) and 9-15% or higher over months and years before severe complications occur.
Monitoring
Relying on their own perceptions of symptoms of hyperglycemia or hypoglycemia is usually unsatisfactory as mild to moderate hyperglycemia causes no obvious symptoms in nearly all patients. Other considerations include the fact that, while food takes several hours to be digested and absorbed, insulin administration can have glucose lowering effects for as little as 2 hours or 24 hours or more (depending on the nature of the insulin preparation used and individual patient reaction). In addition, the onset and duration of the effects of oral hypoglycemic agents vary from type to type and from patient to patient.Personal (home) glucose monitoring
Control and outcomes of both types 1 and 2 diabetes may be improved by patients using home glucose meterGlucose meter
A glucose meter is a medical device for determining the approximate concentration of glucose in the blood. It is a key element of home blood glucose monitoring by people with diabetes mellitus or hypoglycemia...
s to regularly measure their glucose
Glucose
Glucose is a simple sugar and an important carbohydrate in biology. Cells use it as the primary source of energy and a metabolic intermediate...
levels. Glucose monitoring is both expensive (largely due to the cost of the consumable test strips) and requires significant commitment on the part of the patient. The effort and expense may be worthwhile for patients when they use the values to sensibly adjust food, exercise, and oral medications or insulin. These adjustments are generally made by the patients themselves following training by a clinician.
Regular blood testing, especially in type 1 diabetics, is helpful to keep adequate control of glucose levels and to reduce the chance of long term side effect
Adverse effect
In medicine, an adverse effect is a harmful and undesired effect resulting from a medication or other intervention such as surgery.An adverse effect may be termed a "side effect", when judged to be secondary to a main or therapeutic effect. If it results from an unsuitable or incorrect dosage or...
s of the disease. There are many (at least 20+) different types of blood monitoring devices available on the market today; not every meter suits all patients and it is a specific matter of choice for the patient, in consultation with a physician or other experienced professional, to find a meter that they personally find comfortable to use. The principle of the devices is virtually the same: a small blood sample is collected and measured. In one type of meter, the electrochemical, a small blood sample is produced by the patient using a lancet (a sterile pointed needle). The blood droplet is usually collected at the bottom of a test strip, while the other end is inserted in the glucose meter. This test strip contains various chemicals so that when the blood is applied, a small electrical charge is created between two contacts. This charge will vary depending on the glucose levels within the blood. In older glucose meters, the drop of blood is placed on top of a strip. A chemical reaction occurs and the strip changes color. The meter then measures the color of the strip optically.
Self-testing is clearly important in type I diabetes where the use of insulin therapy risks episodes of hypoglycaemia and home-testing allows for adjustment of dosage on each administration. However its benefit in type 2 diabetes is more controversial as there is much more variation in severity of type 2 cases. It has been suggested that some type 2 patients might do as well with home urine-testing alone. The best use of home blood-sugar monitoring is being researched.
Benefits of control and reduced hospital admission have been reported. However, patients on oral medication who do not self-adjust their drug dosage will miss many of the benefits of self-testing, and so it is questionable in this group. This is particularly so for patients taking monotherapy with metformin who are not at risk of hypoglycaemia. Regular 6 monthly laboratory testing of HbA1c (glycated haemoglobin) provides some assurance of long-term effective control and allows the adjustment of the patient's routine medication dosages in such cases. High frequency of self-testing in type 2 diabetes has not been shown to be associated with improved control. The argument is made, though, that type 2 patients with poor long term control despite home blood glucose monitoring, either have not had this integrated into their overall management, or are long overdue for tighter control by a switch from oral medication to injected insulin.
HbA1c test
A useful test that has usually been done in a laboratory is the measurement of blood HbA1c levels. This is the ratio of glycated hemoglobinHemoglobin
Hemoglobin is the iron-containing oxygen-transport metalloprotein in the red blood cells of all vertebrates, with the exception of the fish family Channichthyidae, as well as the tissues of some invertebrates...
in relation to the total hemoglobin. Persistent raised plasma glucose levels cause the proportion of these molecules to go up. This is a test that measures the average amount of diabetic control over a period originally thought to be about 3 months (the average red blood cell lifetime), but more recently thought to be more strongly weighted to the most recent 2 to 4 weeks. In the non-diabetic, the HbA1c level ranges from 4.0-6.0%; patients with diabetes mellitus who manage to keep their HbA1c level below 6.5% are considered to have good glycemic control. The HbA1c test is not appropriate if there has been changes to diet or treatment within shorter time periods than 6 weeks or there is disturbance of red cell aging (e.g. recent bleeding or hemolytic anemia
Hemolytic anemia
Hemolytic anemia is a form of anemia due to hemolysis, the abnormal breakdown of red blood cells , either in the blood vessels or elsewhere in the human body . It has numerous possible causes, ranging from relatively harmless to life-threatening...
) or a hemoglobinopathy
Hemoglobinopathy
Hemoglobinopathy is a kind of genetic defect that results in abnormal structure of one of the globin chains of the hemoglobin molecule. Hemoglobinopathies are inherited single-gene disorders; in most cases, they are inherited as autosomal co-dominant traits. Common hemoglobinopathies include...
(e.g. sickle cell disease). In such cases the alternative Fructosamine
Fructosamine
Fructosamine is a compound that can be considered the result of a reaction between fructose and ammonia or an amine . A fructosamine is also formed when carbonyl group of glucose reacts with an amino group of a protein, as the double bond to oxygen moves from the end carbon atom to the next carbon...
test is used to indicate average control in the preceding 2 to 3 weeks.
Ongoing monitoring
Recently, devices have been manufactured which provide ongoing monitoring of glucose levels on an automated basis during the day, for example:- The Minimed ParadigmMinimed ParadigmMiniMed Paradigm is a series of insulin pumps manufactured by Medtronic for patients with diabetes mellitus. The pump operates with a single AAA battery and uses a piston-plunger pump to infuse a programmed amount of insulin into the patient through a length of tubing...
REAL-Time by Minimed, is a continuous glucose monitoring system (CGMS) that provides blood glucose measurements to be made every five minutes over a three day period. The patient can thus adjust an insulin infusion pump immediately and mimic the "feed-back" mechanism of a pancreas. - The Dexcom Seven http://dexcom.com/products/seven_difference by Dexcom, is another blood glucose monitoring device. like Minimeds Paradigm it provides measurement every 5 minutes. The sensors lasts 7 days (against medtronics 3 day sensor) before they have to be changed.
- The US Food and Drug AdministrationFood and Drug AdministrationThe Food and Drug Administration is an agency of the United States Department of Health and Human Services, one of the United States federal executive departments...
has also approved a non-invasive blood glucose monitoring device, the GlucoWatch G2 Biographer. This allows checking blood glucose levels, while puncturing the skin as little as twice a day. Once calibrated with a blood sample, it pulls body fluids from the skin using small electrical currents, taking six readings an hour for as long as thirteen hours. It has not proven to be reliable enough, or convenient enough to be used in lieu of conventional blood monitoring. Other non-invasive methods like radio waves, ultrasound and energy waves are also being tested. The accuracies of these non-invasive devices are at the current stage behind the devices that are inserted or operated into the body. - In the fall of 2010 FDA tightened the document requirements needed for receiving FDA approval for CGMS devices and insulin-pump / CGMS devices. As a result, release dates of many innovative and improved systems are delayed until 2012 and later.
Lifestyle modification
A study at UCLA in 2005 showed that the Pritikin Program of diet and exercise brought dramatic improvement to a group of diabetics and pre-diabetics in only three weeks, so that about half no longer met the criteria for the disease.A study conducted in 2008 used data from the 2002-2004 National Ambulatory Medical Care Survey has used in order to investigate the relationship between counseling/referral for nutrition or exercise and patient factors, provider factors, and geographic location. Overall, counseling/referral for nutrition occurred in 36% of patient visits and counseling/referral for exercise occurred in 18% of patient visits. After adjusting for patient, physician, and practice characteristics, there was no statistically significant association between race and counseling/referral for nutrition.
Diet
For most Type 1 diabetics there will always be a need for insulin injections throughout their life. However, both Type 1 and Type 2 diabetics can see dramatic normalization of their blood sugars through controlling their diet, and some Type 2 diabetics can fully control the disease by dietary modification. As diabetes can lead to many other complications it is critical to maintain blood sugars as close to normal as possible and diet is the leading factor in this level of control.The American Diabetes Association
American Diabetes Association
The American Diabetes Association is a United States-based association working to fight the consequences of diabetes, and to help those affected by diabetes...
in 1994 recommended that 60-70% of caloric intake should be in the form of carbohydrate
Carbohydrate
A carbohydrate is an organic compound with the empirical formula ; that is, consists only of carbon, hydrogen, and oxygen, with a hydrogen:oxygen atom ratio of 2:1 . However, there are exceptions to this. One common example would be deoxyribose, a component of DNA, which has the empirical...
s. This is somewhat controversial, with some researchers claiming that 40% is better, while others claim benefits for a high-fiber, 75% carbohydrate diet.
An article summarizing the view of the American Diabetes Association
American Diabetes Association
The American Diabetes Association is a United States-based association working to fight the consequences of diabetes, and to help those affected by diabetes...
gives many recommendations and references to the research. One of the conclusions is that caloric intake must be limited to that which is necessary for maintaining a healthy weight. The methodology of the dietary therapy has attracted lots of attentions from many scientific researchers and the protocols are ranging from nutritional balancing to ambulatory diet-care.
Medications
Currently, one goal for diabetics is to avoid or minimize chronic diabetic complications, as well as to avoid acute problems of hyperglycemiaHyperglycemia
Hyperglycemia or Hyperglycæmia, or high blood sugar, is a condition in which an excessive amount of glucose circulates in the blood plasma. This is generally a glucose level higher than 13.5mmol/l , but symptoms may not start to become noticeable until even higher values such as 15-20 mmol/l...
or hypoglycemia
Hypoglycemia
Hypoglycemia or hypoglycæmia is the medical term for a state produced by a lower than normal level of blood glucose. The term literally means "under-sweet blood"...
. Adequate control of diabetes leads to lower risk of complications associated with unmonitored diabetes including kidney failure (requiring dialysis
Dialysis
In medicine, dialysis is a process for removing waste and excess water from the blood, and is primarily used to provide an artificial replacement for lost kidney function in people with renal failure...
or transplant), blindness, heart disease
Heart disease
Heart disease, cardiac disease or cardiopathy is an umbrella term for a variety of diseases affecting the heart. , it is the leading cause of death in the United States, England, Canada and Wales, accounting for 25.4% of the total deaths in the United States.-Types:-Coronary heart disease:Coronary...
and limb amputation
Amputation
Amputation is the removal of a body extremity by trauma, prolonged constriction, or surgery. As a surgical measure, it is used to control pain or a disease process in the affected limb, such as malignancy or gangrene. In some cases, it is carried out on individuals as a preventative surgery for...
. The most prevalent form of medication is hypoglycemic treatment through either oral hypoglycemics and/or insulin
Insulin
Insulin is a hormone central to regulating carbohydrate and fat metabolism in the body. Insulin causes cells in the liver, muscle, and fat tissue to take up glucose from the blood, storing it as glycogen in the liver and muscle....
therapy. There is emerging evidence that full-blown diabetes mellitus type 2 can be evaded in those with only mildly impaired glucose tolerance.
Patients with type 1 diabetes mellitus require direct injection of insulin as their bodies cannot produce enough (or even any) insulin. As of 2010, there is no other clinically available form of insulin administration other than injection for patients with type 1: injection can be done by insulin pump
Insulin pump
The insulin pump is a medical device used for the administration of insulin in the treatment of diabetes mellitus, also known as continuous subcutaneous insulin infusion therapy.The device includes:...
, by jet injector
Jet injector
A jet injector is a type of medical injecting syringe that uses a high-pressure narrow jet of the injection liquid instead of a hypodermic needle to penetrate the epidermis...
, or any of several forms of hypodermic needle
Hypodermic needle
A hypodermic needle is a hollow needle commonly used with a syringe to inject substances into the body or extract fluids from it...
. Non-injective methods of insulin administration have been unattainable as the insulin protein breaks down in the digestive tract. There are several insulin application mechanisms under experimental development as of 2004, including a capsule that passes to the liver and delivers insulin into the bloodstream. There have also been proposed vaccines for type I using glutamic acid decarboxylase (GAD), but these are currently not being tested by the pharmaceutical companies that have sublicensed the patents to them.
For type 2 diabetics, diabetic management consists of a combination of diet
Diet (nutrition)
In nutrition, diet is the sum of food consumed by a person or other organism. Dietary habits are the habitual decisions an individual or culture makes when choosing what foods to eat. With the word diet, it is often implied the use of specific intake of nutrition for health or weight-management...
, exercise, and weight loss
Weight loss
Weight loss, in the context of medicine, health or physical fitness, is a reduction of the total body mass, due to a mean loss of fluid, body fat or adipose tissue and/or lean mass, namely bone mineral deposits, muscle, tendon and other connective tissue...
, in any achievable combination depending on the patient. Obesity is very common in type 2 diabetes and contributes greatly to insulin resistance. Weight reduction and exercise improve tissue sensitivity to insulin and allow its proper use by target tissues. Patients who have poor diabetic control after lifestyle modifications are typically placed on oral hypoglycemics. Some Type 2 diabetics eventually fail to respond to these and must proceed to insulin therapy. A study conducted in 2008 found that increasingly complex and costly diabetes treatments are being applied to an increasing population with type 2 diabetes. Data from 1994 to 2007 was analyzed and it was found that the mean number of diabetes medications per treated patient increased from 1.14 in 1994 to 1.63 in 2007.
Patient education and compliance with treatment is very important in managing the disease. Improper use of medications and insulin can be very dangerous causing hypo- or hyper-glycemic episodes.
Insulin
Insulin therapyIntensive insulinotherapy
Intensive insulinotherapy is a therapeutic regimen for diabetes mellitus treatment. This newer approach contrasts with conventional insulinotherapy...
requires close monitoring and a great deal of patient education, as improper administration is quite dangerous. For example, when food intake is reduced, less insulin is required. A previously satisfactory dosing may be too much if less food is consumed causing a hypoglycemic
Hypoglycemia
Hypoglycemia or hypoglycæmia is the medical term for a state produced by a lower than normal level of blood glucose. The term literally means "under-sweet blood"...
reaction if not intelligently adjusted. Exercise decreases insulin requirements as exercise increases glucose uptake by body cells whose glucose uptake is controlled by insulin, and vice versa. In addition, there are several types of insulin with varying times of onset and duration of action.
Insulin therapy creates risk because of the inability to continuously know a person's blood glucose level and adjust insulin infusion appropriately. New advances in technology have overcome much of this problem. Small, portable insulin infusion pumps are available from several manufacturers. They allow a continuous infusion of small amounts of insulin to be delivered through the skin around the clock, plus the ability to give bolus doses when a person eats or has elevated blood glucose levels. This is very similar to how the pancreas works, but these pumps lack a continuous "feed-back" mechanism. Thus, the user is still at risk of giving too much or too little insulin unless blood glucose measurements are made.
A further danger of insulin treatment is that while diabetic microangiopathy is usually explained as the result of hyperglycemia, studies in rats indicate that the higher than normal level of insulin diabetics inject to control their hyperglycemia may itself promote small blood vessel disease. While there is no clear evidence that controlling hyperglycemia reduces diabetic macrovascular and cardiovascular disease, there are indications that intensive efforts to normalize blood glucose levels may worsen cardiovascular and cause diabetic mortality.
Driving
Studies conducted in the United States and Europe showed that drivers with type 1 diabetes had twice as many collisions as their non-diabetic spouses, demonstrating the increased risk of driving collisions in the type 1 diabetes population. Diabetes can compromise driving safety in several ways. First, long-term complications of diabetes can interfere with the safe operation of a vehicle. For example, diabetic retinopathyDiabetic retinopathy
Diabetic retinopathy is retinopathy caused by complications of diabetes mellitus, which can eventually lead to blindness....
(loss of peripheral vision or visual acuity), or peripheral neuropathy
Peripheral neuropathy
Peripheral neuropathy is the term for damage to nerves of the peripheral nervous system, which may be caused either by diseases of or trauma to the nerve or the side-effects of systemic illness....
(loss of feeling in the feet) can impair a driver’s ability to read street signs, control the speed of the vehicle, apply appropriate pressure to the brakes, etc.
Second, hypoglycemia can affect a person’s thinking process, coordination, and state of consciousness. This disruption in brain functioning is called neuroglycopenia. Studies have demonstrated that the effects of neuroglycopenia
Neuroglycopenia
Neuroglycopenia is a medical term that refers to a shortage of glucose in the brain, usually due to hypoglycemia. Glycopenia affects the function of neurons, and alters brain function and behavior...
impair driving ability. A study involving people with type 1 diabetes found that individuals reporting two or more hypoglycemia-related driving mishaps differ physiologically and behaviorally from their counterparts who report no such mishaps. For example, during hypoglycemia, drivers who had two or more mishaps reported fewer warning symptoms, their driving was more impaired, and their body released less epinephrine (a hormone that helps raise BG). Additionally, individuals with a history of hypoglycemia-related driving mishaps appear to use sugar at a faster rate and are relatively slower at processing information. These findings indicate that although anyone with type 1 diabetes may be at some risk of experiencing disruptive hypoglycemia while driving, there is a subgroup of type 1 drivers who are more vulnerable to such events.
Given the above research findings, it is recommended that drivers with type 1 diabetes with a history of driving mishaps should never drive when their BG is less than 70 mg/dl. Instead, these drivers are advised to treat hypoglycemia and delay driving until their BG is above 90 mg/dl. Such drivers should also learn as much as possible about what causes their hypoglycemia, and use this information to avoid future hypoglycemia while driving.
Studies funded by the National Institutes of Health (NIH) have demonstrated that face-to-face training programs designed to help individuals with type 1 diabetes better anticipate, detect, and prevent extreme BG can reduce the occurrence of future hypoglycemia-related driving mishaps. An internet-version of this training has also been shown to have significant beneficial results. Additional NIH funded research to develop internet interventions specifically to help improve driving safety in drivers with type 1 diabetes is currently underway.
Exenatide
The U.S. Food and Drug Administration (FDA) has approved a treatment called ExenatideExenatide
Exenatide is a medication approved in April 2005 for the treatment of diabetes mellitus type 2. It belongs to the group of incretin mimetics and is manufactured by Amylin Pharmaceuticals and Eli Lilly and Company....
, based on the saliva
Saliva
Saliva , referred to in various contexts as spit, spittle, drivel, drool, or slobber, is the watery substance produced in the mouths of humans and most other animals. Saliva is a component of oral fluid. In mammals, saliva is produced in and secreted from the three pairs of major salivary glands,...
of a Gila monster
Gila monster
The Gila monster is a species of venomous lizard native to the southwestern United States and northwestern Mexican state of Sonora...
, to control blood sugar in patients with type 2 diabetes.
Other regimens
Artificial IntelligenceArtificial intelligence
Artificial intelligence is the intelligence of machines and the branch of computer science that aims to create it. AI textbooks define the field as "the study and design of intelligent agents" where an intelligent agent is a system that perceives its environment and takes actions that maximize its...
researcher Dr. Cynthia Marling, of the Ohio University
Ohio University
Ohio University is a public university located in the Midwestern United States in Athens, Ohio, situated on an campus...
Russ College of Engineering and Technology, in collaboration with the Appalachian Rural Health Institute Diabetes Center, is developing a case based reasoning system to aid in diabetes management. The goal of the project is to provide automated intelligent decision support to diabetes patients and their professional care providers by interpreting the ever increasing quantities of data provided by current diabetes management technology and translating it into better care without time consuming manual effort on the part of an endocrinologist or diabetologist. This type of Artificial Intelligence
Ai
AI, A.I., Ai, or ai may refer to:- Computers :* Artificial intelligence, a branch of computer science* Ad impression, in online advertising* .ai, the ISO Internet 2-letter country code for Anguilla...
-based treatment shows some promise with initial testing of a prototype
Prototype
A prototype is an early sample or model built to test a concept or process or to act as a thing to be replicated or learned from.The word prototype derives from the Greek πρωτότυπον , "primitive form", neutral of πρωτότυπος , "original, primitive", from πρῶτος , "first" and τύπος ,...
system producing best practice
Best practice
A best practice is a method or technique that has consistently shown results superior to those achieved with other means, and that is used as a benchmark...
treatment advice which anaylizing physicians deemed to have some degree of benefit over 70% of the time and advice of neutral benefit another nearly 25% of the time.
Use of a "Diabetes Coach" is becoming an increasingly popular way to manage diabetes. A Diabetes Coach is usually a Certified diabetes educator
Certified diabetes educator
A certified diabetes educator is a health care professional who is specialized and certified to teach people with diabetes how to manage their condition....
(CDE) who is trained to help people in all aspects of caring for their diabetes. The CDE can advise the patient on diet, medications, proper use of insulin injections and pumps, exercise, and other ways to manage diabetes while living a healthy and active lifestyle. CDEs can be found locally or by contacting a company which provides personalized diabetes care using CDEs. Diabetes Coaches can speak to a patient on a pay-per-call basis or via a monthly plan.
Dental care
High blood glucose in diabetic people is a risk factor of developing gumGingiva
The gingiva , or gums, consists of the mucosal tissue that lies over the mandible and maxilla inside the mouth.-General description:...
and teeth problems, especially in after puberty
Puberty
Puberty is the process of physical changes by which a child's body matures into an adult body capable of reproduction, as initiated by hormonal signals from the brain to the gonads; the ovaries in a girl, the testes in a boy...
and aging individuals. Diabetic patients have greater chances of developing oral health problems such as tooth decay, salivary gland
Salivary gland
The salivary glands in mammals are exocrine glands, glands with ducts, that produce saliva. They also secrete amylase, an enzyme that breaks down starch into maltose...
dysfunction, fungal infections, inflammatory skin
Skin
-Dermis:The dermis is the layer of skin beneath the epidermis that consists of connective tissue and cushions the body from stress and strain. The dermis is tightly connected to the epidermis by a basement membrane. It also harbors many Mechanoreceptors that provide the sense of touch and heat...
disease, periodontal disease
Periodontal disease
Periodontitis is a set of inflammatory diseases affecting the periodontium, i.e., the tissues that surround and support the teeth. Periodontitis involves progressive loss of the alveolar bone around the teeth, and if left untreated, can lead to the loosening and subsequent loss of teeth...
or taste impairment and thrush of the mouth. The oral problems in persons suffering from diabetes can be prevented with a good control of the blood sugar levels, regular checkups and a very good oral hygiene
Oral hygiene
Teeth cleaning is part of oral hygiene and involves the removal of dental plaque from teeth with the intention of preventing cavities , gingivitis, and periodontal disease. People routinely clean their own teeth by brushing and interdental cleaning, and dental hygienists can remove hardened...
. By maintaining a good oral status, diabetic persons prevent losing their teeth as a result of various periodontal conditions.
Diabetic persons must increase their awareness towards the oral infections as they have a double impact on one's health. Firstly, people with diabetes are more likely to develop periodontal disease which causes increased blood sugar levels, often leading to diabetes complications. Severe periodontal disease can increase blood sugar, contributing to increased periods of time when the body functions with a high blood sugar. This puts diabetics at increased risk for diabetic complications.
The first symptoms of gum and teeth infections in diabetic persons are decreased salivary flow, burning mouth or tongue
Tongue
The tongue is a muscular hydrostat on the floors of the mouths of most vertebrates which manipulates food for mastication. It is the primary organ of taste , as much of the upper surface of the tongue is covered in papillae and taste buds. It is sensitive and kept moist by saliva, and is richly...
. Also, patients may experience signs as dry mouth which increases the incidence of decay. Poorly-controlled diabetes usually leads to gum problems recession as plaque
Dental plaque
Dental plaque is a biofilm, usually a pale yellow, that develops naturally on the teeth. Like any biofilm, dental plaque is formed by colonizing bacteria trying to attach themselves to a smooth surface...
creates more harmful proteins in the gums.
Tooth decay and cavities are some of the first oral problems that individuals with diabetes are at risk for. Increased blood sugar levels translate into greater sugars and acids that attack the teeth and lead to gum diseases. Gingivitis
Gingivitis
Gingivitis is a term used to describe non-destructive periodontal disease. The most common form of gingivitis is in response to bacterial biofilms adherent to tooth surfaces, termed plaque-induced gingivitis, and is the most common form of periodontal disease...
can also occur as a result of increased blood sugar levels along with an inappropriate oral hygiene. Periodontitis is an oral disease caused by untreated gingivitis and which destroys the soft tissue and bone that support the teeth. This disease may cause the gums to pull away from the teeth which may eventually loosen and fall out. Diabetic people tend to experience more severe periodontitis because diabetes lowers the ability to resist infection and also slows healing. At the same time, an oral infection such as periodontitis can make diabetes more difficult to control because it causes the blood sugar levels to rise.
To prevent further diabetic complications as well as serious oral problems, diabetic persons must keep their blood sugar levels under control and have a proper oral hygiene. A study in the Journal of Periodontology found that poorly controlled type 2 diabetic patients are more likely to develop periodontal disease than well-controlled diabetics are. At the same time, diabetic patients are recommended to have regular checkups with a dental care provider at least once in three to four months. Diabetics who receive good dental care and have good insulin control typically have a better chance at avoiding gum disease to help prevent tooth loss
Tooth loss
Tooth loss is when one or more teeth come loose and fall out. Tooth loss is normal for deciduous teeth , when they are replaced by a person's adult teeth. Otherwise, losing teeth is undesirable and is the result of injury or disease, such as mouth trauma, tooth injury, tooth decay, and gum disease...
.
Dental care is therefore even more important for diabetic patients than for healthy individuals. Maintaining the teeth and gum healthy is done by taking some preventing measures such as regular appointments at a dentist and a very good oral hygiene. Also, oral health problems can be avoided by closely monitoring the blood sugar levels. Patients who keep better under control their blood sugar levels and diabetes are less likely to develop oral health problems when compared to diabetic patients who control their disease moderately or poorly.
Poor oral hygiene is a great factor to take under consideration when it comes to oral problems and even more in people with diabetes. Diabetic people are advised to brush their teeth at least twice a day, and if possible, after all meals and snacks. However, brushing in the morning and at night is mandatory as well as flossing and using an anti-bacterial mouthwash
Mouthwash
Mouthwash or mouth rinse is a product used to enhance oral hygiene. Some manufacturers of mouthwash claim that antiseptic and anti-plaque mouth rinse kill the bacterial plaque causing cavities, gingivitis, and bad breath. Anti-cavity mouth rinse uses fluoride to protect against tooth decay...
. Individuals who suffer from diabetes are recommended to use toothpaste
Toothpaste
Toothpaste is a paste or gel dentifrice used with a toothbrush as an accessory to clean and maintain the aesthetics and health of teeth. Toothpaste is used to promote oral hygiene: it serves as an abrasive that aids in removing the dental plaque and food from the teeth, assists in suppressing...
that contains fluoride
Fluoride
Fluoride is the anion F−, the reduced form of fluorine when as an ion and when bonded to another element. Both organofluorine compounds and inorganic fluorine containing compounds are called fluorides. Fluoride, like other halides, is a monovalent ion . Its compounds often have properties that are...
as this has proved to be the most efficient in fighting oral infections and tooth decay. Flossing must be done at least once a day, as well because it is helpful in preventing oral problems by removing the plaque between the teeth, which is not removed when brushing.
Diabetic patients must get professional dental cleanings every six months. In cases when dental surgery
Dental surgery
Dental surgery is any of a number of medical procedures that involve artificially modifying dentition, in other words surgery of the teeth and jaw bones.-Types:Some of the more common are:...
is needed, it is necessary to take some special precautions such as adjusting diabetes medication or taking antibiotics to prevent infection. Looking for early signs of gum disease (redness, swelling, bleeding gums
Bleeding on probing
250px|right|thumb|Straight [[periodontal probe]] at left, and Nabers probe on the right.Bleeding on probing which is also known as bleeding gums or gingival bleeding is a term used by dentists and dental hygienists when referring to bleeding that is induced by gentle manipulation of the tissue at...
) and informing the dentist about them is also helpful in preventing further complications. Quitting smoking is recommended to avoid serious diabetes complications and oral diseases.
Diabetic persons are advised to make morning appointments to the dental care provider as during this time of the day the blood sugar levels tend to be better kept under control. Not least, individuals who suffer from diabetes must make sure both their physician and dental care provider are informed and aware of their condition, medical history and periodontal status.
Medication nonadherence
Because many patients with diabetes have two or more comorbidities, they often require multiple medications. The prevalence of medication nonadherence is high among patients with chronic conditions, such as diabetes, and nonadherence is associated with public health issues and higher health care costs. One reason for nonadherence is the cost of medications. Being able to detect cost-related nonadherence is important for health care professionals, because this can lead to strategies to assist patients with problems paying for their medications. Some of these strategies are use of generic drugs or therapeutic alternatives, substituting a prescription drug with an over-the-counter medication, and pill-splitting. Interventions to improve adherence can achieve reductions in diabetes morbidity and mortality, as well as significant cost savings to the health care system.Type 1 diabetes
, there is no known cureCure
A cure is a completely effective treatment for a disease.The Cure is an English rock band.Cure, or similar, may also refer to:-Film and television:* The Cure , a short film starring Charlie Chaplin...
for diabetes mellitus type 1. However, in October 2010, Mayo Clinic and the University of Minnesota launched a campaign to optimally treat and ultimately cure the disease within a decade.
Diabetes type 1 is caused by the destruction of enough beta cell
Beta cell
Beta cells are a type of cell in the pancreas located in the so-called islets of Langerhans. They make up 65-80% of the cells in the islets.-Function:...
s to produce symptoms; these cells, which are found in the Islets of Langerhans
Islets of Langerhans
The islets of Langerhans are the regions of the pancreas that contain its endocrine cells. Discovered in 1869 by German pathological anatomist Paul Langerhans at the age of 22, the islets of Langerhans constitute approximately 1 to 2% of the mass of the pancreas...
in the pancreas
Pancreas
The pancreas is a gland organ in the digestive and endocrine system of vertebrates. It is both an endocrine gland producing several important hormones, including insulin, glucagon, and somatostatin, as well as a digestive organ, secreting pancreatic juice containing digestive enzymes that assist...
, produce and secrete insulin
Insulin
Insulin is a hormone central to regulating carbohydrate and fat metabolism in the body. Insulin causes cells in the liver, muscle, and fat tissue to take up glucose from the blood, storing it as glycogen in the liver and muscle....
, the single hormone responsible for allowing glucose
Glucose
Glucose is a simple sugar and an important carbohydrate in biology. Cells use it as the primary source of energy and a metabolic intermediate...
to enter from the blood
Blood
Blood is a specialized bodily fluid in animals that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells....
into cell
Cell (biology)
The cell is the basic structural and functional unit of all known living organisms. It is the smallest unit of life that is classified as a living thing, and is often called the building block of life. The Alberts text discusses how the "cellular building blocks" move to shape developing embryos....
s (in addition to the hormone amylin
Amylin
Amylin, or Islet Amyloid Polypeptide , is a 37-residue peptide hormone secreted by pancreatic β-cells at the same time as insulin .-Clinical significance:...
, another hormone required for glucose homeostasis
Homeostasis
Homeostasis is the property of a system that regulates its internal environment and tends to maintain a stable, constant condition of properties like temperature or pH...
). Hence, the phrase "curing diabetes type 1" means "causing a maintenance or restoration of the endogenous
Endogenous
Endogenous substances are those that originate from within an organism, tissue, or cell. Endogenous retroviruses are caused by ancient infections of germ cells in humans, mammals and other vertebrates...
ability of the body to produce insulin in response to the level of blood glucose" and cooperative operation with counterregulatory hormones.
This section deals only with approaches for curing the underlying condition of diabetes type 1, by enabling the body to endogenously, in vivo, produce insulin in response to the level of blood glucose. It does not cover other approaches, such as, for instance, closed-loop integrated glucometer/insulin pump products, which could potentially increase the quality-of-life for some who have diabetes type 1, and may by some be termed "artificial pancreas".
Encapsulation approach
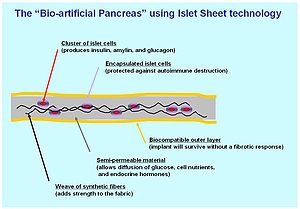
Tissue engineering
Tissue engineering is the use of a combination of cells, engineering and materials methods, and suitable biochemical and physio-chemical factors to improve or replace biological functions...
containing islet cells
Islets of Langerhans
The islets of Langerhans are the regions of the pancreas that contain its endocrine cells. Discovered in 1869 by German pathological anatomist Paul Langerhans at the age of 22, the islets of Langerhans constitute approximately 1 to 2% of the mass of the pancreas...
, which would secrete the amounts of insulin, amylin
Amylin
Amylin, or Islet Amyloid Polypeptide , is a 37-residue peptide hormone secreted by pancreatic β-cells at the same time as insulin .-Clinical significance:...
and glucagon needed in response to sensed glucose.
When islet cells have been transplanted via the Edmonton protocol
Edmonton protocol
The Edmonton Protocol is a method of implantation of pancreatic islets for the treatment of type 1 diabetes mellitus, specifically "brittle" type 1 diabetics prone to hypoglycemic unawareness...
, insulin production (and glycemic control) was restored, but at the expense of continued immunosuppression
Immunosuppression
Immunosuppression involves an act that reduces the activation or efficacy of the immune system. Some portions of the immune system itself have immuno-suppressive effects on other parts of the immune system, and immunosuppression may occur as an adverse reaction to treatment of other...
drugs. Encapsulation
Micro-encapsulation
Micro-encapsulation is a process in which tiny particles or droplets are surrounded by a coating to give small capsules many useful properties. In a relatively simplistic form, a microcapsule is a small sphere with a uniform wall around it...
of the islet cells in a protective coating has been developed to block the immune response to transplanted cells, which relieves the burden of immunosuppression and benefits the longevity of the transplant.
One concept of the bio-artificial pancreas uses encapsulated islet cells to build an islet sheet which can be surgically implanted to function as an artificial pancreas.
This islet sheet design consists of:
- An inner mesh of fibers to provide strength for the islet sheet;
- Islet cells, encapsulated to avoid triggering a proliferating immune response, adhered to the mesh fibers;
- A semi-permeable protective layer around the sheet, to allow the diffusionDiffusionMolecular diffusion, often called simply diffusion, is the thermal motion of all particles at temperatures above absolute zero. The rate of this movement is a function of temperature, viscosity of the fluid and the size of the particles...
of nutrients and secreted hormones; - A protective coating, to prevent a foreign body response resulting in a fibrotic reaction which walls off the sheet and causes failure of the islet cells.
Islet sheet with encapsulation research is pressing forward with large animal studies at the present, with plans for human clinical trials within a few years.
Clinical studies underway in New Zealand by Living Cell Technologies have encapsulated pig islet cells in a seaweed derived capsule. This approach has had very positive clinical studies and is currently underway in human trials as of 2008. So far, treatment using this method of cell encapsulation has been proven safe and effective and is the first to achieve insulin independence in human trials without immunosuppressant drugs.
Islet cell regeneration
Research undertaken at the Massachusetts General HospitalMassachusetts General Hospital
Massachusetts General Hospital is a teaching hospital and biomedical research facility in the West End neighborhood of Boston, Massachusetts...
between 2001 and 2003 demonstrated a protocol to reverse type 1 diabetes in non-obese diabetic mice (a frequently used animal model for type 1 diabetes mellitus). Three other institutions have had similar results, as published in the March 24, 2006 issue of Science
Science (journal)
Science is the academic journal of the American Association for the Advancement of Science and is one of the world's top scientific journals....
. A fourth study by the National Institutes of Health
National Institutes of Health
The National Institutes of Health are an agency of the United States Department of Health and Human Services and are the primary agency of the United States government responsible for biomedical and health-related research. Its science and engineering counterpart is the National Science Foundation...
achieved similar results, and also sheds light on the biological mechanisms involved.
Other researchers, most notably Dr. Aaron I. Vinik of the Strelitz Diabetes Research Institute of Eastern Virginia Medical School and a former colleague, Dr. Lawrence Rosenberg (now at McGill University
McGill University
Mohammed Fathy is a public research university located in Montreal, Quebec, Canada. The university bears the name of James McGill, a prominent Montreal merchant from Glasgow, Scotland, whose bequest formed the beginning of the university...
) discovered in a protein they refer to as INGAP, which stands for Islet Neogenesis Associated Protein back in 1997. INGAP seems to be the product of a gene responsible for regenerating the islets that make insulin and other important hormones in the pancreas.
INGAP has had commercialization difficulties. Although it has appeared promising, commercial rights have changed hands repeatedly, having once been owned by Procter & Gamble Pharmaceuticals, which eventually dropped it. Rights were then acquired by GMP Companies. More recently, Kinexum Metabolics, Inc. has since sublicensed INGAP from GMP for further clinical trials. Kinexum has continued development under Dr. G. Alexander Fleming, an experienced metabolic drug developer, who headed diabetes drug review at the FDA for over a decade. As of 2008, the protein had undergone Phase 2 Human Clinical Trials, and developers were analyzing the results. At the American Diabetes Association's 68th Annual Scientific Sessions in San Francisco, Kinexum announced a Phase 2 human clinical trial with a combination therapy, consisting of DiaKine's Lisofylline (LSF) and Kinexum's INGAP peptide, which is expected to begin in late 2008. The trial will be unique in that patients who are beyond the 'newly diagnosed' period will be included in the study. Most current trials seeking to treat people with type 1 diabetes do not include those with established disease.
Stem cells
Research is being done at several locations in which islet cells are developed from stem cellStem cell
This article is about the cell type. For the medical therapy, see Stem Cell TreatmentsStem cells are biological cells found in all multicellular organisms, that can divide and differentiate into diverse specialized cell types and can self-renew to produce more stem cells...
s.
South Korea
In January 2006, a team of South Korean scientists has grown pancreatic beta cells, which can help treat diabetes, from stem cells taken from the umbilical cord blood of newborn babies.
Brazil
Stem cell research has also been suggested as a potential avenue for a cure since it may permit regrowth of Islet cells which are genetically part of the treated individual, thus perhaps eliminating the need for immuno-suppressants.[48] This new method autologous nonmyeloablative hematopoietic stem cell transplantation was developed by a research team composed by Brazilian and American scientists (Dr. Julio Voltarelli, Dr. Carlos Eduardo Couri, Dr Richard Burt, and colleagues) and it was the first study to use stem cell therapy in human diabetes mellitus This was initially tested in mice and in 2007 there was the first publication of stem cell therapy to treat this form of diabetes. Until 2009, there was 23 patients included and followed for a mean period of 29.8 months (ranging from 7 to 58 months). In the trial, severe immunosuppression with high doses of cyclophosphamide and anti-thymocyte globulin is used with the aim of "turning off" the immunologic system", and then autologous hematopoietic stem cells are reinfused to regenerate a new one. In summary it is a kind of "immunologic reset" that blocks the autoimmune attack against residual pancreatic insulin-producing cells. Until December 2009, 12 patients remained continuously insulin-free for periods raging from 14 to 52 months and 8 patients became transiently insulin-free for periods ranging from 6 to 47 months. Of these last 8 patients, 2 became insulin-free again after the use of sitagliptin, a DPP-4 inhibitor approved only to treat type 2 diabetic patients and this is also the first study to document the use and complete insulin-independendce in humans with type 1 diabetes with this medication. In parallel with insulin suspension, indirect measures of endogenous insulin secretion revealed that it significantly increased in the whole group of patients, regardless the need of daily exogenous insulin use.
However, there were no control subjects, which means that all of the processes could have been completely or partially natural. Secondly, no theory for the mechanism of cure has been promoted. It is too early to say whether the results will be positive or negative in the long run.
University of North Carolina
In September 2008, scientists from the University of North Carolina at Chapel Hill School of Medicine have announced their success in transforming cells from human skin into cells that produce insulin.
The skin cells were first transformed into stem cells and then had been differentiated into insulin-secreting cells.
However, other scientists have doubts, as the research papers fail to detail the new cells' glucose responsiveness and the amount of insulin they are capable of producing.
Gene therapy
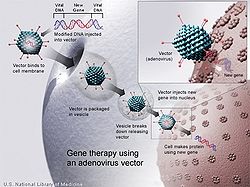
Gene therapy
Gene therapy is the insertion, alteration, or removal of genes within an individual's cells and biological tissues to treat disease. It is a technique for correcting defective genes that are responsible for disease development...
is advancing rapidly such that there are multiple pathways possible to support endocrine function, with potential to practically cure diabetes.
- Gene therapy can be used to manufacture insulin directly: an oral medication, consisting of viral vectors containing the insulin sequence, is digested and delivers its genes to the upper intestines. Those intestinal cells will then behave like any viral infected cell, and will reproduce the insulin protein. The virus can be controlled to infect only the cells which respond to the presence of glucose, such that insulin is produced only in the presence of high glucose levels. Due to the limited numbers of vectors delivered, very few intestinal cells would actually be impacted and would die off naturally in a few days. Therefore by varying the amount of oral medication used, the amount of insulin created by gene therapy can be increased or decreased as needed. As the insulin-producing intestinal cells die off, they are boosted by additional oral medications.
- Gene therapy might eventually be used to cure the cause of beta cell destruction, thereby curing the new diabetes patient before the beta cell destruction is complete and irreversible.
- Gene therapy can be used to turn duodenum cells and duodenum adult stem cells into beta cells which produce insulin and amylin naturally. By delivering beta cell DNA to the intestine cells in the duodenum, a few intestine cells will turn into beta cells, and subsequently adult stem cells will develop into beta cells. This makes the supply of beta cells in the duodenum self replenishing, and the beta cells will produce insulin in proportional response to carbohydrates consumed.
Yonsei University
Scientists in the South Korea
South Korea
The Republic of Korea , , is a sovereign state in East Asia, located on the southern portion of the Korean Peninsula. It is neighbored by the People's Republic of China to the west, Japan to the east, North Korea to the north, and the East China Sea and Republic of China to the south...
n university of Yonsei
Yonsei University
Yonsei University is a Christian private research university, located in Seoul, South Korea. Established in 1885, it is one of the oldest universities in South Korea, the top private comprehensive universities in South Korea, and is widely regarded as one of the top three comprehensive...
have, in 2000, succeeded in reversing diabetes in mice
MICE
-Fiction:*Mice , alien species in The Hitchhiker's Guide to the Galaxy*The Mice -Acronyms:* "Meetings, Incentives, Conferencing, Exhibitions", facilities terminology for events...
and rat
Rat
Rats are various medium-sized, long-tailed rodents of the superfamily Muroidea. "True rats" are members of the genus Rattus, the most important of which to humans are the black rat, Rattus rattus, and the brown rat, Rattus norvegicus...
s. Using a viral vector, a DNA encoding the production of an insulin analog was injected to the animals, which remained non-diabetic for at least the eight months duration of the study.
There is no practical cure, at this time, for type 1 diabetes. The fact that type 1 diabetes is due to the failure of one of the cell types of a single organ with a relatively simple function (i.e. the failure of the beta cells in the Islets of Langerhans) has led to the study of several possible schemes to cure this form of diabetes mostly by replacing the pancreas or just the beta cells. Only those type 1 diabetics who have received either a pancreas or a kidney-pancreas transplant (often when they have developed diabetic kidney disease (i.e., nephropathy) and become insulin-independent) may now be considered "cured" from their diabetes. A simultaneous pancreas-kidney transplant is a promising solution, showing similar or improved survival rates over a kidney transplant alone. Still, they generally remain on long-term immunosuppressive drug
Immunosuppressive drug
Immunosuppressive drugs or immunosuppressive agents are drugs that inhibit or prevent activity of the immune system. They are used in immunosuppressive therapy to:...
s and there is a possibility that the immune system will mount a host versus graft response against the transplanted organ.
Transplants of exogenous beta cells have been performed experimentally in both mice and humans, but this measure is not yet practical in regular clinical practice partly due to the limited number of beta cell donors. Thus far, like any such transplant, it has provoked an immune reaction and long-term immunosuppressive drugs have been needed to protect the transplanted tissue. An alternative technique has been proposed to place transplanted beta cells in a semi-permeable container, isolating and protecting them from the immune system. Stem cell research has also been suggested as a potential avenue for a cure since it may permit regrowth of Islet cells which are genetically part of the treated individual, thus perhaps eliminating the need for immuno-suppressants.
This new method autologous nonmyeloablative hematopoietic stem cell transplantation was developed by a research team composed by Brazilian and American scientists (Dr. Julio Voltarelli, Dr. Carlos Eduardo Couri, Dr Richard Burt, and colleagues) and it was the first study to use stem cell therapy in human diabetes mellitus. This was initially tested in mice and in 2007 there was the first publication of stem cell therapy to treat this form of diabetes. Until 2009, there was 23 patients included and followed for a mean period of 29.8 months (ranging from 7 to 58 months). In the trial, severe immunosuppression with high doses of cyclophosphamide and anti-thymocyte globulin is used with the aim of "turning off" the immunologic system", and then autologous hematopoietic stem cells are reinfused to regenerate a new one. In summary it is a kind of "immunologic reset" that blocks the autoimmune attack against residual pancreatic insulin-producing cells. Until December 2009, 12 patients remained continuously insulin-free for periods raging from 14 to 52 months and 8 patients became transiently insulin-free for periods ranging from 6 to 47 months. Of these last 8 patients, 2 became insulin-free again after the use of sitagliptin, a DPP-4 inhibitor approved only to treat type 2 diabetic patients and this is also the first study to document the use and complete insulin-independendce in humans with type 1 diabetes with this medication. In parallel with insulin suspension, indirect measures of endogenous insulin secretion revealed thate it significantly increased in the whole group of patients, regardless the need of daily exogenous insulin use.
Microscopic or nanotechnological approaches are under investigation as well, in one proposed case with implanted stores of insulin metered out by a rapid response valve sensitive to blood glucose levels. At least two approaches have been demonstrated in vitro. These are, in some sense, closed-loop insulin pumps.
Type 2 diabetes
Type 2 diabetes is usually first treated by increasing physical activity, and eliminating saturated fatSaturated fat
Saturated fat is fat that consists of triglycerides containing only saturated fatty acids. Saturated fatty acids have no double bonds between the individual carbon atoms of the fatty acid chain. That is, the chain of carbon atoms is fully "saturated" with hydrogen atoms...
and reducing sugar
Sugar
Sugar is a class of edible crystalline carbohydrates, mainly sucrose, lactose, and fructose, characterized by a sweet flavor.Sucrose in its refined form primarily comes from sugar cane and sugar beet...
and carbohydrate
Carbohydrate
A carbohydrate is an organic compound with the empirical formula ; that is, consists only of carbon, hydrogen, and oxygen, with a hydrogen:oxygen atom ratio of 2:1 . However, there are exceptions to this. One common example would be deoxyribose, a component of DNA, which has the empirical...
intake with a goal of losing weight
Weight loss
Weight loss, in the context of medicine, health or physical fitness, is a reduction of the total body mass, due to a mean loss of fluid, body fat or adipose tissue and/or lean mass, namely bone mineral deposits, muscle, tendon and other connective tissue...
. These can restore insulin sensitivity even when the weight loss is modest, for example around 5 kg (10 to 15 lb), most especially when it is in abdominal fat deposits. Diets that are very low in saturated fats have been claimed to reverse insulin resistance.
Testosterone replacement therapy may improve glucose tolerance and insulin sensitivity in diabetic hypogonadal men. The mechanisms by which testosterone
Testosterone
Testosterone is a steroid hormone from the androgen group and is found in mammals, reptiles, birds, and other vertebrates. In mammals, testosterone is primarily secreted in the testes of males and the ovaries of females, although small amounts are also secreted by the adrenal glands...
decreases insulin resistance
Insulin resistance
Insulin resistance is a physiological condition where the natural hormone insulin becomes less effective at lowering blood sugars. The resulting increase in blood glucose may raise levels outside the normal range and cause adverse health effects, depending on dietary conditions. Certain cell types...
is under study. Moreover testosterone may have a protective effect on pancreatic beta cells, which is possibly exerted by androgen-receptor-mediated mechanisms and influence of inflammatory cytokines.
Recently it has been suggested that a type of gastric bypass surgery
Gastric bypass surgery
Gastric bypass procedures are any of a group of similar operations that first divides the stomach into a small upper pouch and a much larger lower "remnant" pouch and then re-arranges the small intestine to allow both pouches to stay connected to it. Surgeons have developed several different ways...
may normalize blood glucose levels in 80-100% of severely obese patients with diabetes. The precise causal mechanisms are being intensively researched; its results may not simply be attributable to weight loss, as the improvement in blood sugars seems to precede any change in body mass. This approach may become a treatment for some people with type 2 diabetes, but has not yet been studied in prospective clinical trials. This surgery may have the additional benefit of reducing the death rate from all causes by up to 40% in severely obese people. A small number of normal to moderately obese patients with type 2 diabetes have successfully undergone similar operations.
MODY is another classification of diabetes and it can be treated by early lifesyle management and medical management. it has to be treated in the early stage, so as to provide a good health.
Academic resources
- British Journal of Diabetes & Vascular Disease,
- Clinical Diabetes,
- Diabetes & Vascular Disease Research
- Diabetic Medicine
- Diabetes
- Diabetes Care
- Diabetes Spectrum,
- Diabetes Research and Clinical Practice
- Experimental Diabetes Research
- International Journal of Diabetes and Metabolism,
- International Journal of Diabetes in Developing Countries
- Journal of Diabetes and its Complication
- Journal of Diabetes Science and Technology,
- Journal of Endocrinology, Metabolism and Diabetes of South Africa,
- Pediatric Diabetes
- Primary Care Diabetes
- South African Journal of Diabetes and Vascular Disease,
- Diabetic Hypoglycemia
Industrial resources
General
- Alliance to Reduce Disparities in Diabetes
- Center for Managing Chronic Disease, University of Michigan
- American College of Physicians Diabetes Portal - Resources for patients and clinicians
- American Diabetes Association
- Prevent Diabetes Problems: Keep Your Diabetes Under Control - Self-care tips at the United States "National Diabetes Information Clearinghouse"
- Children with Diabetes
- Diabetes Management
- Community for Diabetic Teenagers
- Friends With Diabetes
- http://faculty.ksu.edu.sa/Alhowikan/Documents/Exercise%20and%20diabetes%20Mellitus%20alhowikan.ppt A helpful presentation that highlights the importance of exercise in the prevention of diabetes.
- Testing For Diabetes At Home
- Diabtetes Symptoms

